Auriculotherapy for low back pain in primary health care: systematic review
Introduction
Low back pain (LBP) is one of the most widespread public health problems worldwide, affecting 60% to 80% of the population (1). The largest apparent increase in disability caused by LBP in recent decades is in low- and middle-income countries, including Asia, Africa and the Middle East (2). In primary health care (PHC), LBP is among the most prevalent pain conditions (3), generating a great demand for the health system, becoming costly for both the individual and society (4,5).
The LBP is nonspecific in the great majority of cases and this type of LBP occurs when there is no suspicion or confirmation of primary disease, or known cause such as a tumor, fracture, osteoporosis and radicular syndrome (6). In this context, treatment focuses on reducing pain and its consequences through pharmacological and non-pharmacological approaches, such as education and exercise. However, overuse of drugs can be a problem, as with opioids (7). In this sense, complementary practices can reduce the medicalization of care, promote the importance of subjectivity of the subjects, and bring new alternatives of actions with the use of less expensive and more adequate resources for comprehensive care of the human being (8).
Auriculotherapy (AT)—an application of physical stimuli in specific auricular points—may be a potential strategy to face the challenges that LBP brings to the health system and society since studies have shown promising results in its application in the LBP management, with reduced pain intensity and improved functionality (4,5). The objective of this article is to present the results of a literature systematic review (SR) conducted to support the development of a clinical recommendation for the use of AT for the LBP management in PHC based on evidence. This recommendation is inserted in a context of continuing education within a broader project of elaboration of AT recommendations for common and relevant clinical conditions in PHC; to be used in its most synthetic version by the almost 10 thousand professionals of the Unified Health System (SUS) who took the AT course offered by the Federal University of Santa Catarina, sponsored by the Brazilian Ministry of Health (9,10).
We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/lcm-21-31).
Methods
The present SR was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (11), although it has not been registered in SR databases, such as PROSPERO for example. Searches were conducted in 15 databases: PubMed/MEDLINE; EMBASE; Scopus; Web of Science; PsycINFO; PEDro (Physiotherapy Evidence Database); Cochrane Database of Systematic Reviews; Cochrane Central Register of Controlled Trials; CNKI; Clinicaltrials.gov; CINAHL; LILACS; Virtual Health Library on Traditional, Complementary and Integrative Medicines-BVS MTCI; OASIS Brasil and two grey literature databases: ProQuest Dissertations & Theses Global and Open Grey Database.
The descriptors used were a combination of descriptors as sensitive as possible for the terms similar to “auriculotherapy”, “and” “low back pain”. The descriptors are shown in detail in Table 1.
Table 1
| Database | Search strategy | Number of retrieved references |
|---|---|---|
| PubMed/Medline | (“auriculotherapy”[MeSH Terms] OR Auricul* OR “Acupuncture, Ear”[Mesh] OR “ear acupuncture” OR “ear acupressure” OR ((“acupressure”[MeSH Terms] OR “acupressure” OR “pellet” OR “pellets” OR “point” OR “points” OR “seed” OR “seeds” OR “plaster” OR “plasters” OR “Semen Vaccariae” OR “Sinapis alba” OR “Acupoint” OR “acupoints” OR “acupuncture points”[MeSH Terms]) AND (“Ear”[Mesh:NoExp] OR “ear” OR “ears”))) AND (“Back Pain”[Mesh:NoExp] OR “Low back pain”[Mesh] OR “LBP” OR “Back Pain”[Title/Abstract] OR “Back Pains” OR “Backache” OR “Backaches” OR “Back Ache” OR “Back Aches” OR “Sciatica” OR “low back pain” OR “lumbargo” OR “lumbarlgia” OR “lumbosacral” OR “dorsalgia” OR “Spine”[Mesh:NoExp] OR “Spine”[Title/Abstract] OR “spinal pain”) AND (English[lang] OR Portuguese[lang] OR Spanish[lang]) | 183 |
| Embase | 313 | |
| Scopus | 403 | |
| Web of Science | 191 | |
| CINAHL | 72 | |
| Cochrane Database of Systematic Reviews (CDSR) | 0 | |
| Cochrane Central Register of Controlled Trials (CENTRAL) | 108 | |
| PsycINFO | 12 | |
| PEDro (Physiotherapy Evidence Database) | 31 | |
| CNKI (China National Knowledge Infrastructure) | 2 | |
| Clinical trials.gov | 4 | |
| LILACS | 41 | |
| Virtual Health Library on Traditional, Complementary and Integrative Medicines (Biblioteca Virtual em Saúde em Medicinas Tradicionais, Complementares e Integrativas) (BVS MTCI)) | 27 | |
| Oasisbr (Open Access and Scholarly Information System) | 16 | |
| ProQuest Dissertations & Theses Global | 7 | |
| Open Grey | 1 | |
| Total | 1,411 | |
The database searches were carried out by an experienced librarian on March 4th, 2020, and exported to Endnote-web bibliographic management software to eliminate duplicates. They were then exported to Rayyan (12), an application developed by Qatar Computing Research Institute (QCRI), for document selection in the SR development.
Inclusion criteria were as follows: RCT and non-RCTs with parallel groups or in crossover or SR format with or without meta-analysis, published in English, Portuguese or Spanish languages were included. Studies that compared AT and its variations as monotherapy, with at least one control group (CG) using no treatment, placebo treatment, sham treatment or usual drug or behavioral treatment that was effective within the context of Western medicine. Acceptable variations of AT were considered: auriculopressure with seeds or spheres (semmen vaccaria, magnetic spheres, among others) and AT withholding needles (semipermanent). In addition to clinical trials, SRs were included when they considered evaluations of AT efficacy independently of other therapies and were accepted for their potential to broaden the empirical basis of the recommendation by including publications in other languages, especially Eastern languages.
The following exclusion criteria were used: protocol studies, research projects, non-comparative studies (case series and case studies); observational studies of the before-and-after type and other observational studies; studies that used AT techniques in the format of AT sessions without retention stimulus; and studies in which there was only a comparison between different AT techniques (e.g., AT using magnetic spheres versus AT using Vaccaria seeds), since this type of comparison does not allow an evaluation of the AT effectiveness.
The studies were selected as follows: first, an experienced librarian extracted the publications from the databases and excluded duplicates. Subsequently, the titles and abstracts of all publications were independently analyzed for inclusion criteria by two reviewers to eliminate irrelevant publications and possible remaining duplicates. Then, the full texts of the possibly relevant studies were read in their entirety by the same two reviewers independently. At each step, the reviewers confronted the results and either consented to discrepancies or, when necessary, a third reviewer contributed to the final decision. The reviewers were not blinded to the authors’ names, institutions, or the journal of publication of each study.
The same two reviewers extracted the data from the included studies and conducted the quality assessment of these articles independently. All conflicts of judgment were settled by consensus.
The following data were extracted from the analyzed studies: article reference, main study population characteristics (e.g., age, sex, ethnicity, comorbidities, disease status, outpatient/inpatient setting), inclusion and exclusion criteria, sample number, study design, which comparisons were carried out, a treatment protocol of the experimental group (EG) (including stimulus time, number of sessions, treatment time, the material used, points used in the EG), a treatment protocol of the CG(s), follow-up time, outcome measures, a summary of results.
The quality of included studies was assessed using checklists developed by the Scottish Intercollegiate Guidelines Network, version 2019 (13) for RCTs and RSs.
Results
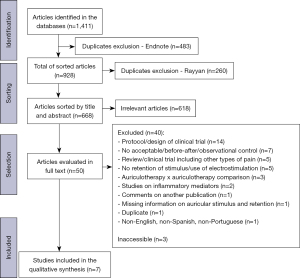
Of the 1,411 documents identified by systematic searches in the researched databases, 668 were left for analysis after the elimination of duplicates. Of these 668, only 50 were selected for full-text analysis, and three of these were not located for reading in full. Therefore, 47 publications were analyzed, of which seven articles were included, six of them RCTs and one SR. The flowchart in Figure 1 describes the screening and selection process.
Study characteristics and summary of findings
The RCTs’ samples ranged from 21 to 200 participants, with an average of 91 participants per study, and were published between 2009 and 2019. The SR analyzed included seven RCTs published between 2007 and 2015, among which three are part of the RCTs analyzed individually in this study.
RCTs’ participants were recruited from different places. In only two of the six included RCTs, participants were recruited directly from PHC services. In the other RCTs, participants were recruited through flyers distributed in practices, health centers, at the university, etc. Although these were not PHC services, the community context of recruitment seems to make the participants’ profiles compatible with PHC users. In five of the six included RCTs, the mean ages of the participants were computed and are 31, 41, 42, 63 and 73 years. In one RCT, the age ranged from 20 to 70 years. In all studies, the minimum age of the participants considered was 18 years.
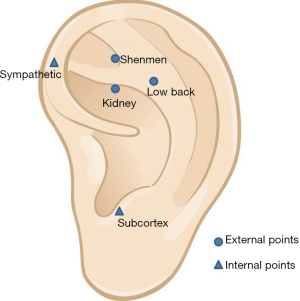
The time of the studies ranged from 2 to 4 weeks, with weekly treatment frequency. In three of the six included RCTs, holding needles were used on the points specific to EGs and nonspecific to CGs. In the other three RCTs, spherical vegetable seeds adhered to the points were used and participants were instructed to press the seeds 3 times a day for 3 minutes each time. The main points used in these studies in the EGs were: shenmen, subcortex, sympathetic, kidney and lumbar (Figure 2).
Characteristics of the SR
The selected SR presented a meta-analysis of 7 RCTs involving a total of 369 participants described as adults with chronic LBP, with various comparison groups (placebo, other complementary or conventional therapies), in which 15 auricular points receiving auricular stimulation via auricular needles were used (5). The meta-analysis showed that auricular acupuncture had a large and significant effect on pain relief within 4 weeks [SMD =−0.78, 95% CI, (−1.22, −0.33), P<0.001] (Table 2).
Table 2
| Article | Number of articles and types of study | Sample size and characteristics | Comparisons made | Points used and main ones | Stimulation patterns | Summary of the conclusions |
|---|---|---|---|---|---|---|
| Yang et al. (5) | 7 RCTs | SR of RCTs that included 369 adult patients with chronic LBP |
Of the 7 RCTs, 4 used the auricle vs. placebo comparison. The remaining studies used Tai Chi exercise/conventional medicine/stretched twist walking training as a comparison | In all included studies, 15 auricular acupuncture points were used. Shenmen and subcortex were the frequently used auricular points, considered primarily for pain relief, followed by lumbosacral region, liver, kidney, sympathetic, lumbar, waist, popliteal fossa, posterior spinal sulcus, sciatic nerve, urinary bladder, buttock, spleen and Ashi point, respectively | Unavailable | EG showed statistically significant improvement regarding pain relief at 4 weeks of AT when compared to CG [SMD =−0.78, 95% CI, (−1.22, −0.33), P<0.001] |
SR, systematic review; RCTs, randomized clinical trials; LBP, low back pain; EG, experimental group; CG, control group; SMD, standardized mean difference; CI, confidence interval.
Characteristics of RCTs
In all six included RCTs, presented in Table 3, the pain was assessed as the primary endpoint, with a disability, functionality, quality of life, beliefs, anxiety, coping and medication use as secondary endpoints, assessed respectively through the instruments: Roland Morris Disability Questionnaire (RMDQ) (14-17) Oswestry Disability Questionnaire (ODQ) (14), International Physical Activity Questionnaire (IPAQ), Quality of Life Questionnaire (EQ-5D) (14), Fear Avoidance Beliefs Questionnaire (FABQ) (4-17); visual analog scale (VAS) (16), disability rating index (DRI) (16), Short Pain Intensity-short form (BPI-sf) (4,16-18), McGill Short Form Pain Questionnaire (MPQ-SF) (16,17), MPI-s (4-16), general anxiety disorder (16-17), The Pain and Catastrophizing Scale (PCS) (4,16,17), Quality of Life Assessment Instrument—WHO (WHOQOL-BREF) (4) and Medication Quantification Score—Version III (MQS III) (17).
Table 3
| Article | Participants’ context and characteristics | Sample dropout (%) | EG (intervention number) | CG (intervention number) | Duration | Outcome | Results | Used points |
|---|---|---|---|---|---|---|---|---|
| Hunter et al. (14) | Participants with chronic (Z3 mo) or recurrent (Z3 episodes in the previous 12 months) LBP of mechanical origin with/without radiation in the buttocks and thighs (synonymous with mechanical LBP) |
17% EG |
N=24 |
N=27 |
12 weeks | ODQ, |
EG showed improvement concerning |
Shenmen, lumbar spine |
| Vas et al. (15) | Pregnant women 24 to 36 weeks gestation aged 18 years or older diagnosed with pregnancy-related LBPGP who have not received prior acupuncture treatment | 6.8% |
N=55 |
G2—n=55 |
2 weeks | VAS |
Reduction of pain intensity in the |
G1—shenmen and kidney and at a reflex point in the region of the ear that classically represents the lumbar or sacral regions |
| Wang et al. (16) | Healthy pregnant women of ASA physical status II, with no previous experience with acupuncture, gestational age 25–38 weeks, with low back and/or posterior pelvic pain | 4.4% | N=54 |
N=58 |
2 weeks | EVA-P DRI | Significant differences in pain in the groups: 37% in EG and 22% in CG |
Kidney, anemia, shenmen |
| Yeh et al. (17) | Older adults over 65 years of age of white race |
26% EG |
N=19 |
N=18 |
4 weeks | BPI-sf |
The reduction in worst pain from baseline to end of intervention was 41% for EG |
EG: shenmen, sympathetic subcortex, and points for LBP in the posterior region |
| Yeh et al. (4) | Age 18 years or older; had CLBP defined as LBP of at least three months duration and reported a mean pain intensity score related only to their CLB ≥4 on a numeric number from 0 to 10 point pain scale in the past week | 10% EG |
N=11 |
N=10 |
4 weeks | BPI-sf |
Participants in the EG who completed the 4-week treatment had a 70% reduction in worst pain intensity, a 75% reduction in overall pain intensity, and a 42% improvement in disability due to back pain at the initial assessment |
EG: shenmen, sympathetic subcortex, and points for LBP in the posterior region |
| Yeh et al. (18) | The mean age was 63.3 years (SD 5 16.70; range, |
17% EG |
N=30 |
N=31 |
4 weeks | BPI-sf |
The greatest improvement shown |
EG: shenmen, sympathetic and nervous subcortex |
RCTs, randomized clinical trials; EG, experimental group; CG, control group; LBP, low back pain; AT, auriculotherapy; ODQ, Oswestry Disability Questionnaire; EQ-5D, Quality of Life Questionnaire; RMDQ, Roland Morris Disability Questionnaire; IPAQ, International Physical Activity Questionnaire; FABQ, Fear Avoidance Beliefs Questionnaire; CI, confidence interval; LBPGP, lower back and/or posterior pelvic girdle pain; SOC, standard obstetric care; VEA, verum ear acupuncture; VAS, visual analog scale; SF-12, Short Form-12 Health Survey; ASA, American Society of Anesthesiologists; DRI, disability rating index; BPI-sf, Short Pain Intensity-short; MPQ-SF, McGill Pain Questionnaire Short Form; GAD-7, general anxiety disorder; PCS, The Pain and Catastrophizing Scale; WHOQOL-BREF, Quality of Life Assessment Instrument—from WHO; APA, auricular point acupressure; MQS III, Medication Quantification Scoring—Version III; DPC, daily percent change.
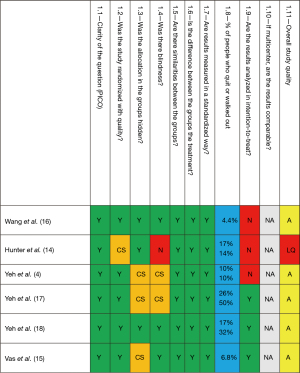
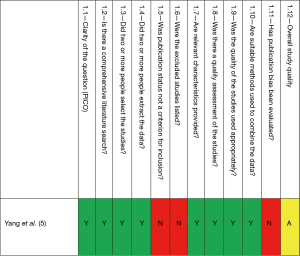
In all six RCTs that were evaluated (Table 3), there was a positive effect of AT in the EGs, which showed significant advantages over the CGs. Of the six selected RCTs, five were evaluated as acceptable quality (A), although two of them had a high dropout percentage, and one was evaluated as low quality (LQ) (14) because it provided little information about the methodological procedures. As for the only SR included, this was evaluated as of A. Therefore, overall, six of seven included publications are of A, as can be seen in Figures 3,4.
Of the five RCTs that received an A evaluation, we highlight the small 2013 pilot trial conducted by researchers (4) for the level of result they achieved. In this study, there was a comparison between a real AT group and a non-specific point group (sham group). The former received Vaccaria seed at the points: shenmen, sympathetic, subcortex and lumbar. The sham group received stimulation on the points: stomach, kidney, duodenum and mouth. Four sessions were carried out with analysis one month after the end of the treatment. Participants in the true AT group who completed the treatment had a 70% reduction in worst pain intensity, a 75% reduction in overall pain intensity, and a 42% improvement in disability due to back pain compared to the initial assessment. The reductions in the worst pain and overall pain intensity in the intervention group were statistically greater than participants in the CG (P<0.01) at the end of four weeks and after 1 month of follow-up. The authors noted that the outcome of this study exceeded that of previous studies.
If the other four A RCTs, two of them are authored by Yeh, published in consecutive years (17,18), and had clinically significant results, although showing less benefit than the 2013 pilot trial. In 2014, researchers (17) found the following results: the reduction in worst pain from baseline to the end of the intervention was 41% for the true treatment group and 5% for the sham group, with a Cohen’s effect size of 1.22 (P<0.01). Disability scores on the Roland Morris Disability Questionnaire (RMDQ) decreased in the intervention group by 29% and remained unchanged in the CG (+3%) (P<0.01). However, the high percentage of dropouts drew attention when interpreting this result.
In the 2015 study, scientists (18) found the following result: among participants in the intervention group, a 30% reduction in worst pain was achieved after the first day of treatment, and a greater reduction in pain (44%) was reported by this group after completing treatment in 4 weeks. This magnitude of pain reduction reached the clinically significant level of improvement reported in other clinical trials of chronic pain therapies.
Another 2 RCTs (15,16), which had A ratings, worked with pregnant women investigating the effect of auricular acupuncture associated with standard obstetric care (SOC), in primary care, on LBPGP (late lower back and/or posterior pelvic girdle pain) experienced by pregnant women. Both concluded that after 2 weeks of treatment auricular acupuncture applied by midwives and associated with standard obstetric treatment will significantly reduce lumbar and pelvic pain in pregnant women, improve quality of life, and reduce functional disability. It is worth noting that the Vas et al. study is the most recent among those included and also has the largest sample size, with 220 participants.
Discussion
This SR searched 15 databases, including gray literature, RCTs and RSs. Six RCTs with a total of 392 participants and one SR with 369 participants were included, and 3 studies included in this review were part of the studies included among the RCTs.
The search methodology, the diversity of databases and the SR strengthened the sensitivity and specificity of the review, although the language restriction was a limitation. The low number of studies included, compared to the relatively large number of studies extracted from the databases, perhaps due to the common use of AT in association with other conventional and unconventional therapies, with relatively few studies evaluating the effect of AT alone on LBP, which was our focus of interest.
A limitation of our results was that most of the studies analyzed had a short follow-up time for the patients, except for the one study (14), which followed the participants for 12 weeks. For example, in other study (4), although the dropout rate was low (only two participants did not complete the study), there was a small sample size and patients were followed for a short period of time, which may have influenced the results. Therefore, the results of the selected studies should be analyzed with caution and their various limitations, including the percentage of dropout, should not be ignored. The high dropout rate in two trials (17,18) suggests that patients found auricular acupuncture or seed therapy to be uncomfortable and were unwilling to persist with their treatment. It may be that these particular patients felt they were getting no benefit.
We found five studies that were assessed as A and one as BQ, plus one SR of acceptable quality. Quality was assessed using valid scripts (Scottish Intercollegiate Guidelines Network) (13) directed to the development of clinical guidelines (Figures 3,4), which allow the classification of studies concerning how well the study was conducted to minimize biases. Since they are tools proposed for guideline construction, they consider clinical and methodological aspects and the statistical power of the study to determine the degree of certainty that the overall effect is due to the intervention evaluated in the study, as well as whether or not the results are directly applicable to the target population of the guidelines (13). Of the six RCTs considered in this review, one was shown to be of LQ, two were conducted on pregnant ladies, and the remaining three were from the same author in successive years. Thus, the combined results are unlikely to be generalizable.
LBP is a complex condition with multiple contributing factors such as overweight, sedentary lifestyle, behavioral and socio-demographic factors like ethnicity, gender, age, education and social status (19,20). Moreover, it is a condition that causes negative impacts on functional capacity, productivity, leading to premature inactivity and bringing significant psychosocial consequences (1,3,21). In this sense, the studies included in our review evaluated, in addition to pain, outcomes such as disability, functionality, quality of life, beliefs, anxiety and catastrophizing.
All studies evaluated the efficacy of auricular therapy alone, with seeds (14-16) or retaining needles (4,17,18), without combining it with other treatments. In general, patients who used the auricular acupressure technique, as opposed to those who used retention needles, were instructed to press the stitches during the week, but did not receive supervision or verification of compliance with this guidance. Overall, the studies did not describe the criteria for choosing the points used in the intervention groups. However, all studies used the lumbar point as a reflex action point in LBP, combined with autonomic action points such as shenmen, sympathetic and subcortex. Only two studies (15,16) used the kidney point, which follows syndromic differentiation criteria by traditional Chinese medicine.
Most of the studies analyzed used non-specific points in the CG as sham points, except for two studies that compared the intervention group with standard therapy (14,15). We emphasize that there is evidence that non-specific points can also have a therapeutic effect on pain control and even in other conditions. Therefore, different points in any region of the ear, such as in the auricular periphery, where innervation of the spinal and trigeminal branches predominates, or points in the auricular center, where innervation of the auricular branch of the vagus nerve predominates, can activate endogenous mechanisms and promote analgesia (22). The use of “sham points” in AT seems not to be inert, which can reduce the difference obtained between the control and intervention groups. This leads to an underestimated outcome bias when studies use sham-AT with stimuli at non-specific points. Also, when it comes to AT, the proximity of the points is quite small. Even so, the use of nonspecific points in the CG is still the most used methodology in clinical studies of AT (22).
Finally, several elements suggest caution: only 6 studies were included (despite the high sensitivity of the search); short follow-up time; few participants; 2 studies with high dropout rates; 3 did not have their results analyzed in intention-to-treat and 3 were from the same author. On the other hand, the 5 acceptable-quality RCTs used sham in the CGs, which systematically minimizes differences in comparisons. And clinically and statistically significant better results were obtained in the EGs of all studies. With these findings, we assess that the overall balance is in favor of AT as an effective complementary treatment, albeit temporarily.
Conclusions
Studies of A suggest that AT is an effective therapy in the treatment of LBP, especially with the use of points such as shenmen, lumbar, kidney, sympathetic and subcortex. However, due to the limitations of the analyzed studies, such results are probably not generalizable and should be evaluated with caution. More robust RCTs should be conducted.
Acknowledgments
We thank Lucio José Botelho, Ari Ocampo Ojeda Moré, João Eduardo Marten Teixeira, Maria Gorete Monteguti Savi, Emiliana Domingues Cunha da Silva and Melissa Costa Santos for the discussions on the methodological design and publications analysis.
Funding: This article was supported by the Brazilian Ministry of Health [201712635], Coordination for the Improvement of Higher Education Personne [88882.437598/2019-01,88882.437589/2019-1,88882437850/2019-01] to [DSN, JRR, MLN] and National Council for Research and Development of Brazil [303999/2018-7] to [CDT].
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Longhua Chinese Medicine for the series “Ear acupuncture neuromodulation”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/lcm-21-31
Peer Review File: Available at https://dx.doi.org/10.21037/lcm-21-31
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/lcm-21-31). The series “Ear acupuncture neuromodulation” was commissioned by the editorial office without any funding or sponsorship. MLN served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Morais ML, Silva VKO, Silva JMN. Prevalence of low back pain and associated factors among physiotherapy students. Br J Pain 2018;1:241-7.
- Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet 2018;391:2356-67. [Crossref] [PubMed]
- Langoni CS, Valmorbida LA, Resende TL. A introdução de atendimentos por fisioterapeutas em unidade de atenção primária em saúde. Rev Bras Prom Saude 2012;25:261-70. [Crossref]
- Yeh CH, Chien LC, Balaban D, et al. A randomized clinical trial of auricular point acupressure for chronic low back pain: a feasibility study. Evid Based Complement Alternat Med 2013;2013:196978 [Crossref] [PubMed]
- Yang LH, Duan PB, Hou QM, et al. Efficacy of Auricular Acupressure for Chronic Low Back Pain: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid Based Complement Alternat Med 2017;2017:6383649 [Crossref] [PubMed]
- Almeida DC, Kraychete DC. Low back pain–a diagnostic approach. Rev Dor 2017;18:173-7. [Crossref]
- Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet 2017;389:736-47. [Crossref] [PubMed]
- Telesi E Jr. Práticas integrativas e complementares em saúde, uma nova eficácia para o SUS. Estud Av 2016;30:99-112. [Crossref]
- Tesser CD, Santos MC, Silva EDC, et al. Capacitação em auriculoterapia para profissionais do SUS de 2016-2017. Revise 2021;5:1-18. [Crossref]
- Tesser CD, Moré AOO, Santos MC, et al. Auriculotherapy in primary health care: A large-scale educational experience in Brazil. J Integr Med 2019;17:302-9. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097 [Crossref] [PubMed]
- Available online: https://rayyan.qcri.org/welcome
- Scottish Intercollegiate Guidelines Network. Sign 50: a guideline developer’s handbook. Edinburgh: SIGN, 2019.
- Hunter RF, McDonough SM, Bradbury I, et al. Exercise and Auricular Acupuncture for Chronic Low-back Pain: A Feasibility Randomized-controlled Trial. Clin J Pain 2012;28:259-67. [Crossref] [PubMed]
- Vas J, Cintado MC, Aranda-Regules JM, et al. Effect of ear acupuncture on pregnancy-related pain in the lower back and posterior pelvic girdle: A multicenter randomized clinical trial. Acta Obstet Gynecol Scand 2019;98:1307-17. [Crossref] [PubMed]
- Wang SM, Dezinno P, Lin EC, et al. Auricular acupuncture as a treatment for pregnant women who have low back and posterior pelvic pain: a pilot study. Am J Obstet Gynecol 2009;201:271.e1-9. [Crossref] [PubMed]
- Yeh CH, Morone NE, Chien LC, et al. Auricular point acupressure to manage chronic low back pain in older adults: a randomized controlled pilot study. Evid Based Complement Alternat Med 2014;2014:375173 [Crossref] [PubMed]
- Yeh CH, Kwai-Ping Suen L, Chien LC, et al. Day-to-Day Changes of Auricular Point Acupressure to Manage Chronic Low Back Pain: A 29-day Randomized Controlled Study. Pain Med 2015;16:1857-69. [Crossref] [PubMed]
- Ferreira GD, Silva MC, Rombaldi AJ, et al. Prevalence and associated factors of back pain in adults from southern Brazil: a population-based study. Rev Bras Fisioter 2011;15:31-6. [Crossref] [PubMed]
- Zanuto EA, Codogno JS, Christófaro DG, et al. Prevalence of low back pain and associated factors in adults from a middle-size Brazilian city. Cien Saude Colet 2015;20:1575-82. [Crossref] [PubMed]
- Malta DC, Oliveira MM, Andrade SSCA, et al. Factors associated with chronic back pain in adults in Brazil. Rev Saude Publica 2017;51:9s. [Crossref] [PubMed]
- Lundeberg T, Lund I, Sing A, et al. Is placebo acupuncture what it is intended to be? Evid Based Complement Alternat Med 2011;2011:932407 [Crossref] [PubMed]
Cite this article as: N’bundé DS, Farias Pelachini FT, Rothstein JR, Neves ML, Tesser CD. Auriculotherapy for low back pain in primary health care: systematic review. Longhua Chin Med 2021;4:37.