Narrative review of evaluation on the effect of traditional Chinese medicine on Alzheimer’s disease via machine learning approaches
Introduction
Alzheimer’s disease (AD), of which the main group of symptoms is the decline in cognitive functions, is a rapidly increasing global public health challenge (1). However, unfortunately, there is still no effective treatment to recover this disease now, so that the main treatments for AD focus on the prevention of the progress in AD and the improvements of the cognitive functions. Meanwhile, traditional Chinese medicine (TCM), which is a group of traditional medical treatments based the ancient Chinese philosophy and is popular in China, may benefit the development of AD treatments: some compounds from TCM herbs can improve the AD patients’ symptoms and TCM healthcare practice may be helpful to reduce the medical burden for AD patients (2,3). However, due to the lack of high-quality trials of TCM treatments for AD, it may be difficult to evaluate the effect of the TCM for AD. But, because of the huge amounts of AD patients taking TCM treatments in China, the ‘real-world evidence’, that refers to medical information from multiple sources including medical records, data from mobile applications and so on, maybe helpful to evaluate the effect and drug safety of TCM for AD (4). And, compared to the traditional statistical methods, the machine learning approaches, commonly focusing on classification and prediction, maybe a more suitable way to analyse the complex and massive dataset of the real world (5). Hence, it is of interest to discuss how to use machine learning approaches to evaluate the effect of TCM for AD. This literature review will just give a general suggestion for this topic, which may be a reference for further researches on this topic. In this review, recent literature will be preferred to include. As a complex topic, in further research, amounts of researchers need to cooperate in the data collection and the development of the process of data analysis in detail to reach the consensus of the suitable research that can determine the effect of TCM for AD. And, this literature review will be divided into two parts. The first part will give a brief introduction to AD, TCM and machine learning. The second part will give the general suggestion about how to build the data set and evaluate the data. We present the following article in accordance with the Narrative Review reporting checklist (available at https://dx.doi.org/10.21037/lcm-20-43).
Background
AD
AD is a chronic progressive neurodegenerative disorder (6). And, there are various conjectures and theories about the cause of AD, such as acceleration of ageing, mutations of amyloid precursor protein (APP) and presenilin (PSEN) genes, and so on (7). AD could be classified into typical AD, atypical AD, mixed AD and preclinical states of AD according to IWG-2 Diagnostic Criteria for AD (8). Among the classifications of AD, typical AD may be the most common AD in the AD population (9), of which the specific clinical phenotype of typical AD is early and significant episodic memory impairment (8). According to the recommendations of USA National Institute on Aging-Alzheimer’s Association workgroups, the progress of AD could be divided into the stages of preclinical AD, mild cognitive impairment (MCI) and AD dementia, and the cognitive functions gradually of patients decrease with AD progress (10).
The incidence of AD is relatively high in the ageing population, and approximately 69.9% of all dementia is due to AD (11). Especially in developed countries with population ageing, AD can give a considerable public health burden. For instance, in 2013, the age-standardised rate of dementia was 7.1% in the ageing population (>65) in the UK and cost about £26.3 billion to the UK society, with an average cost of £32,250 per person (12). And as a prediction based on 2002–2013 data, the number of dementia patients in England and Wales may increase by 57% from 2016 to 2040 (13). Hence, whatever current and future, AD may be a major public health issue for the society with population ageing.
Although there is no cure treatment for AD, drug therapies are recommended in the treatment for AD. For instance, the cholinesterase inhibitors like donepezil could be used in all stages of AD for improving cognition and behaviour functions (14). And, memantine, a kind of N-methyl-D-aspartate (NMDA) receptor, is recommended to be used for patients with moderate-to-severe AD for improving related functions (15). In addition, the diet may also be associated with biomarkers of AD. For instance, the Mediterranean diet and ‘AD protective’ diets (higher intake of fresh fruit and vegetables, whole grains fish, low-fat dairies and so on) could decrease AD biomarker levels in PET images, cerebrospinal fluid and plasma. Meanwhile, since AD is an irreversible neurodegenerative disorder (16), early treatment and care strategies may have a significant effect in delaying the progress of AD.
In summary, as a common chronic progressive neurodegenerative disorder, early treatment and care strategies are critical in the treatments for AD. Hence, the progress of the early stage of AD can be used to evaluate the effect of an intervention.
TCM
TCM, one of the oldest traditional medical systems, includes herbal medicine, acupuncture, massage, food therapy and so on (17). In this system, human health is thought to depend on the normal ‘circulation of Qi (a kind of energy in TCM theory) and blood’ in the human body (17). Currently, this traditional medical system is still accepted by a considerable amount of Chinese and TCM are commonly used in the healthcare system in China. And, among the current TCM treatments, the effect and advantage of TCM herbal medicine may be one of the common controversies. This treatment analyzes the patients’ disorders or diseases based on ‘Wu Xing’ (or ‘Five Elements’), ‘Yin Yang’ or other TCM theories, which can describe their situation into different ‘imbalance’ nature situations. Then, the TCM doctors will give patients the decoction of the combination of the corresponding herbs which can improve the ‘imbalance’. Normally, patients even with the same diseases can describe as different ‘imbalance’ nature situations. Hence, the decoction of the combination and amounts of herbs may also be different for each patient in practice, so that it may be difficult to design the trial with strict inclusion criteria to evaluate the effect of TCM herbs due to this different herb treatment for each patient.
Some researchers try to use evidence-based medicine methods to summarize and gain a stable finding for TCM herbs in different diseases. In evidence-based medicine, systematic review and meta-analysis can be used to gain a stable evaluation of treatment through collecting different trials data in little different settings (18). Though some theories of TCM may be hardly integrated into modern medicine, some evidence-based medicine researchers have found that a treatment strategy containing the combination of modern medicine and TCM may have advantages in the effect of treatments for some diseases to some extent. For instance, a systematic review and meta-analysis of randomized controlled trials (RCTs) illustrated that the combination of acupuncture treatment and conventional treatment may reduce chronic pelvic pain in women with a significantly higher total effectiveness rate (19). However, the lack of high quality often leads to that the researchers may only have very little confidence in their findings. In the area of AD, the situation may be similar. A systematic review and meta-analysis illustrated that ‘acupuncture plus Chinese herbal medicine’ may be more effective at improving the Mini-Mental State Examination (MMSE) score than the modern medical treatment, however, the low quality of those RCTs used in this evidence-based medicine research also gives rise to low confidence in this finding (20). As a result, the low-quality clinical trial for TCM may give a rise to low-quality evidence-based medicine for TCM.
Hence, the current medical evidence in RCTs-evidence-based medicine may hardly evaluate the accurate effect of TCM for AD with high confidence. Meanwhile, the real-world data of TCM clinical practice, that is the main application setting of TCM, can play an important role in the evaluation of the effect of TCM for AD and other diseases (21), where machine learning techniques may be able to give a favour.
Machine learning
Now, precision medicine, an advancing field of medical research was being applied in the optimization of diagnosis and treatment strategies for individuals based on the genomics and biomarkers of patients and diseases (22). For instance, advanced pancreatic cancer patients with different genomic/transcriptomic may have different responses to chemotherapy, which could be the theoretical basis for the further tailored treatment approaches (23). In terms of AD, current precision medical researchers concentrate on the determination of the risk profile of AD, underlying molecular mechanisms (22). For example, the variants of APOE and other common genetic could be used to estimate the risk for AD through a genetic risk score (24). However, the majority of clinical trials about AD ignored the potential clinical and molecular heterogeneity of the disease (22). Meanwhile, the mechanism of AD is not clearly determined, which means that the optimization of treatment strategies only by genetic factors may not be very accurate. And, besides genetic factors, environmental factors such as exposure to aluminium and other factors may also have effects on the risk of AD (7). Therefore, further developments are needed on the optimization of treatment strategies for AD based on diverse characteristics instead of relying solely on genetic data.
Machine learning technology includes a set of methods which allow computers to learn meaningful patterns directly from data without human intervention (25). Nowadays, machine learning is widely applied in the recognition of medical images. For instance, cancer pathological images can be automatically identified as malignant or benign using machine learning techniques (26). For AD, the machine learning approach has been applied in different fields. For example, the artificial neural network (ANN) can help to extracts the hippocampus region from images and detecting AD-based MRI scans (27), and the Support Vector Machines (SVM) method can indicate the whole-genome spectrum of AD based on known gene-gene interaction data (28) and so on. And, in the area of MRI images science, a general process of appeal machine learning is as fellow: (I) pre-processing the MRI scans and extracting features of interesting areas such as texture, shape from the pre-processing MRI scans; (II) feeding the feature vector of the training set to the trained model for classification; (III) verifying the effect of the trained model in the test set. Meanwhile, deep learning (e.g., convolutional neural network), a popular method in computer vision, can detect the features automatically for classification. Currently, in the field of machine learning for AD diagnosis, there are over 100 prominent papers that used ANN and SVM method mainly and built models with accurate performance (29), which illustrate machine learning may currently be a stable technique for AD diagnosis to some extent. Hence, when optimizing the treatment strategies of AD, the image evidence can be an important index to prove if the disease progress has been controlled and the high effect diagnosis model established by machine learning may help to classify the disease progress more accurately to generate the more precise image evidence to assist evaluation. And, the AD Neuroimaging Initiative (ADNI) may be the most common-used database for AD diagnosis machine learning research (30). Hence, it may be a meaningful way for the optimization of treatment strategies for AD by referring to the data of ADNI and a diagnosis tool based the machine learning on this data.
Recently, it was shown that hippocampal radiomic features could be used as predictors of progression from MCI to AD dementia (31). Hence, the change of hippocampal radiomic features may be an index to optimize treatment strategies for patients with AD or preclinical stages of AD. However, to the best of our knowledge, the machine learning method has not been applied in optimizing treatment strategies for patients with AD or preclinical stages of AD based on a model including the effect of changes of hippocampal radiomic features.
In summary, the current machine learning research in AD may just focus on the diagnosis of AD and the development of evaluating the effect of TCM for AD can also benefit the research in evaluating other treatments for AD.
Potential suggestion
As we have mentioned above, TCM may give different treatments for each patient and machine learning techniques may be the potential to optimize the TCM treatments for each patient. This article also considers that evaluate the effect of TCM for AD for each patient may be the initial step to describe the effect of TCM. Hence, we consider training the model to estimate or predict the time length from MIC to AD for each patient taking modern medical treatment only or the combination of TCM treatments and modern medical treatment if the patient took the other treatment strategy.
Data
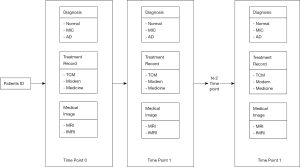
The ADNI is a longitudinal multi-centre study to improve the early detection and tracking of AD, support advances in AD treatments and share data to all scientists in the world (adni.loni.usc.edu/about/). The database of ADNI contains that clinical, genetic and images of normal, MCI and AD subjects. This database includes 2,551 subjects and the subjects of this database are recruited across North America from 2004. Researchers can establish the dataset used to evaluate the effect of TCM for AD by referring to the data structure of this database. Hence, the researchers can have a general structure like Figure 1. Besides, the diagnosis, medical treatment record and image, other records of interest can also be collected. And, both patients only taking modern medical treatment and patients taking the combination of TCM treatments and modern medical treatment will be included. So, by comparing the real-time length and the estimated time length, it may be possible to assess the benefit or the loss of TCM for AD for each variable.
Predictor variables
The main predictor will be the treatment records and medical images. Additionally, another record of interest like social-economic factors can also be considered. By including multi-dimensional factors in training, the model can predict or estimate the time length from MIC to AD accurately for each subject.
Outcome measure
The main outcomes will be the time length from MIC to AD, which can suggest that to what extent the progress of AD can be controlled by medical treatment or the combination of TCM treatments and modern medical treatment. Though the time length from normal to MIC can also be considered to evaluate that to what extent the AD can be prevented by medical treatment or the combination of TCM treatments and modern medical treatment, the patients maybe not likely to take modern medical or TCM treatments for preventing AD intentionally before the diagnosis of MIC. Hence, in this article, we just suggest the time length from MIC to AD as the main outcomes.
Machine learning methods
This article suggests the use of the deep learning method for modelling since it does not require the selection of features of medical images before training. After finished data collection and before modelling, the skull stripping of images, intensity normalization and other data pre-processing or data augmentation techniques will be conducted. At the end of data pre-processing, the data will be split randomly into a training set, a validation set and a test set.
After modelling, we can use the model to estimate or predict the time length from MIC to AD for each patient when the patient takes different treatment strategies. Then, the predicted length will be compared to the real value to evaluate the benefit or the loss of TCM for AD for each subject. And, after evaluating the benefit or the loss of TCM for AD in our dataset, this model can also be used to help determine if the doctor should give a patient the combination of TCM treatments and modern medical treatment in the future clinical practice.
Limitation
Similar to many other machine learning models, one of the main limitations of this model is that this model can only give the predicted value rather than a clear explanation and causality inference. But, for deeply understanding the mechanism of AD and developing the recovery treatment, a clear explanation in biomedical terms is needed. A possible solution for this issue is that we can include the omics data for each subject in the modelling. Through differentiating the omics data for each subject, possible biomedical findings may appear, however, that will lead to additional costs.
Conclusions
The current medical evidence in clinical trials and evidence-based medicine may hardly evaluate the effect of TCM for AD with high confidence. Hence, this review suggests a model evaluating the effect of TCM for AD. However, due to the complexity of AD, this review can only give a general suggestion. Before data collection, further consensus in details under censor between researchers is still needed.
Acknowledgments
Thanks to Mr Xiatian Zhang (University of Southampton, Southampton, SO17 1BJ, UK) for his valuable contribution to inspiring our research.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Longhua Chinese Medicine for the series “Narrative & Evidence-based Medicine for Traditional Medicine: from basic research to clinical practice and trail”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://dx.doi.org/10.21037/lcm-20-43
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/lcm-20-43). The series “Narrative & Evidence-based Medicine for Traditional Medicine: from basic research to clinical practice and trail” was commissioned by the editorial office without any funding or sponsorship. BL served as the unpaid Guest Editor of the series and serves as an unpaid Associate Editor-in-Chief of Longhua Chinese Medicine from March 2021 to February 2023. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Borenstein A, Mortimer J. Alzheimer’s disease: life course perspectives on risk reduction. Academic Press, 2016.
- Lin SK, Lo PC, Chen WC, et al. Integrating traditional Chinese medicine healthcare into dementia care plan by reducing the need for special nursing care and medical expenses. Medicine (Baltimore) 2019;98:e14468 [Crossref] [PubMed]
- Sun ZK, Yang HQ, Chen SD. Traditional Chinese medicine: a promising candidate for the treatment of Alzheimer's disease. Transl Neurodegener 2013;2:6. [Crossref] [PubMed]
- Corrigan-Curay J, Sacks L, Woodcock J. Real-World Evidence and Real-World Data for Evaluating Drug Safety and Effectiveness. JAMA 2018;320:867-8. [Crossref] [PubMed]
- Crown WH. Real-World Evidence, Causal Inference, and Machine Learning. Value Health 2019;22:587-92. [Crossref] [PubMed]
- Burns A, Iliffe S. Alzheimer's disease. BMJ 2009;338:b158. [Crossref] [PubMed]
- Armstrong RA. What causes alzheimer's disease? Folia Neuropathol 2013;51:169-88. [Crossref] [PubMed]
- Dubois B, Feldman HH, Jacova C, et al. Advancing research diagnostic criteria for Alzheimer's disease: the IWG-2 criteria. Lancet Neurol 2014;13:614-29. [Crossref] [PubMed]
- Wang HF, Tan L, Cao L, et al. Application of the IWG-2 Diagnostic Criteria for Alzheimer's Disease to the ADNI. J Alzheimers Dis 2016;51:227-36. [Crossref] [PubMed]
- Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7:280-92. [Crossref] [PubMed]
- Brookmeyer R, Evans DA, Hebert L, et al. National estimates of the prevalence of Alzheimer's disease in the United States. Alzheimers Dement 2011;7:61-73. [Crossref] [PubMed]
- Prince M, Knapp M, Guerchet M, et al. Dementia UK: Update. London: Alzheimer's Society; 2014.
- Ahmadi-Abhari S, Guzman-Castillo M, Bandosz P, et al. Temporal trend in dementia incidence since 2002 and projections for prevalence in England and Wales to 2040: modelling study. BMJ 2017;358:j2856. [Crossref] [PubMed]
- Deardorff WJ, Feen E, Grossberg GT. The Use of Cholinesterase Inhibitors Across All Stages of Alzheimer's Disease. Drugs Aging 2015;32:537-47. [Crossref] [PubMed]
- Grossberg GT, Manes F, Allegri RF, et al. The safety, tolerability, and efficacy of once-daily memantine (28 mg): a multinational, randomized, double-blind, placebo-controlled trial in patients with moderate-to-severe Alzheimer's disease taking cholinesterase inhibitors. CNS Drugs 2013;27:469-78. [Crossref] [PubMed]
- Mendiola-Precoma J, Berumen LC, Padilla K, Garcia-Alcocer G. Therapies for Prevention and Treatment of Alzheimer's Disease. Biomed Res Int. 2016;2016:2589276 [Crossref] [PubMed]
- Tang JL, Liu BY, Ma KW. Traditional Chinese medicine. Lancet 2008;372:1938-40. [Crossref] [PubMed]
- Higgins JP, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, 2019.
- Sung SH, Sung AD, Sung HK, et al. Acupuncture Treatment for Chronic Pelvic Pain in Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid Based Complement Alternat Med 2018;2018:9415897 [Crossref] [PubMed]
- Zhou S, Dong L, He Y, et al. Acupuncture plus Herbal Medicine for Alzheimer's Disease: A Systematic Review and Meta-Analysis. Am J Chin Med 2017;45:1327-44. [Crossref] [PubMed]
- Zhou X, Liu B, Zhang X, et al. Data Mining in Real-World Traditional Chinese Medicine Clinical Data Warehouse. In: Poon J, Poon SK, editors. Data Analytics for Traditional Chinese Medicine Research. Cham: Springer International Publishing; 2014:189-213.
- Reitz C. Toward precision medicine in Alzheimer's disease. Ann Transl Med 2016;4:107. [Crossref] [PubMed]
- Aung KL, Fischer SE, Denroche RE, et al. Genomics-Driven Precision Medicine for Advanced Pancreatic Cancer: Early Results from the COMPASS Trial. Clin Cancer Res 2018;24:1344-54. [Crossref] [PubMed]
- van der Lee SJ, Wolters FJ, Ikram MK, et al. The effect of APOE and other common genetic variants on the onset of Alzheimer's disease and dementia: a community-based cohort study. Lancet Neurol 2018;17:434-44. [Crossref] [PubMed]
- Fu GS, Levin-Schwartz Y, Lin QH, et al. Machine Learning for Medical Imaging. J Healthc Eng 2019;2019:9874591 [Crossref] [PubMed]
- Erickson BJ, Korfiatis P, Akkus Z, et al. Machine Learning for Medical Imaging. Radiographics 2017;37:505-15. [Crossref] [PubMed]
- Raut A, Dalal V. editors. A machine learning based approach for detection of alzheimer’s disease using analysis of hippocampus region from MRI scan. 2017 International Conference on Computing Methodologies and Communication (ICCMC); 2017.
- Huang X, Liu H, Li X, et al. Revealing Alzheimer's disease genes spectrum in the whole-genome by machine learning. BMC Neurol 2018;18:5. [Crossref] [PubMed]
- Tanveer M, Richhariya B, Khan RU, et al. Machine learning techniques for the diagnosis of Alzheimer’s disease: A review. ACM Transactions on Multimedia Computing, Communications, and Applications 2020;16:1-35. [Crossref]
- Vemuri P, Gunter JL, Senjem ML, et al. Alzheimer's disease diagnosis in individual subjects using structural MR images: validation studies. Neuroimage 2008;39:1186-97. [Crossref] [PubMed]
- Zhao K, Ding Y, Han Y, et al. Independent and reproducible hippocampal radiomic biomarkers for multisite Alzheimer’s disease: diagnosis, longitudinal progress and biological basis. Sci Bull 2020;65:1103-13. [Crossref]
Cite this article as: Li B, Lin Y. Narrative review of evaluation on the effect of traditional Chinese medicine on Alzheimer’s disease via machine learning approaches. Longhua Chin Med 2021;4:34.