Short-term efficacy of spinal manipulation in addition to pharmacological treatment of acute low back pain in the emergency department: a randomized controlled trial
Introduction
Low back pain (LBP) is a common condition which may result from a variety of known or unknown etiologies (1). World Health Organisation (WHO) estimates the lifetime prevalence of non-specific LBP to be between 60% and 70% in the modern world (2). LBP is associated with a variety of predisposing factors, including psychological disorders, obesity, smoking, lack of physical activity, age and lifestyle (3).
LBP may be classified by duration as acute (pain lasting less than 6 weeks), sub-chronic (6 to 12 weeks), or chronic (more than 12 weeks) (4). Only about 5% of acute LBP cases present as pain consequent to compression, lumbar disc herniation, spinal stenosis (or narrowing), or epidural fibrosis (5). A majority of the rest of all acute LBP cases are non-specific, meaning that it cannot be attributed to any specific pathology of the spine and is usually associated with muscle spasms (6).
There is a wide acceptance that the management of LBP should begin in primary care (4,7). However, in clinical practice acute LBP is one of the leading complaints encountered in emergency departments (ED) (8). Although emergency medicine may not be considered primary care, it provides some elements of primary care (9) and from the viewpoint of treatments of LBP we see that there are strong interrelations in clinical practice.
There are a variety of available medications for the relief of LBP, all of which come with their own sets of benefits and disadvantages (10). Even though most physicians prescribe non-steroid anti-inflammatory drugs (NSAIDs) to LBP patients, this treatment is often found unsatisfactory, and overuse can lead to many side effects (10). There are also various non-pharmacological methods available for the treatment of LBP such as spinal manipulative therapies or other manual therapies (11).
Physical therapy has been the most commonly preferred treatment method for LBP for a long time (12). The limited use of recommended first-line treatments and improper use of imaging methods, rest, opioids, and invasive interventions are indicators of inadequate LBP treatment (13). On the other hand, patients with LBP are known to resort to various integrative medicine methods, most commonly manipulative therapies.
Manipulative therapies include the treatment of biomechanical problems of the musculoskeletal system through manual manipulation of joints (14). For instance, chiropractic care utilizes the manipulation of both the spine and non-spinal extremities (15). It is a nonpharmacological and noninvasive method (16). Generally, manipulative therapies focus on the manipulation of the spine and related tissues to correct joint alignment problems, alleviate pain, improve function and promote health care (17). Manipulative therapists are trained to evaluate and treat LBP-related musculoskeletal disorders (18). Recent evidence-based clinical guidelines for the management of acute and chronic LBP primarily recommend non-pharmacological approaches for first-line treatment (5). A multimodal approach including spinal manipulation and exercise is considered as an effective treatment strategy for LBP (5). Utilization of manipulative therapies is steadily increasing in the western world (19).
Recently, WHO has urged member states, in accordance with national capacities, priorities, relevant legislation and circumstances to develop and implement, as appropriate, working plans to integrate traditional medicine into health services particularly primary health care services (WHA 67.18) (20). In Turkiye, Regulation on Practices of Traditional and Complementary Medicine (T&CM) entered into force in 2014 (21). This Regulation represents a step to establish legal instruments and clear rules regarding integrative medicine practices that can be performed by the licensed medical doctors after having an add-on training. The Regulation states fifteen separate methods which include manual therapies.
The aim of this study was to investigate the short-term effectiveness of add-on integrative spinal manipulation for acute LBP compared to standard treatment in the emergency department. We present the following article in accordance with the CONSORT reporting checklist (available at https://dx.doi.org/10.21037/lcm-21-11).
Methods
Study design
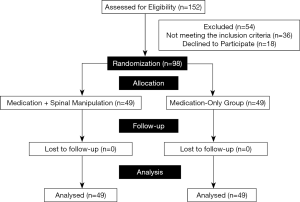
This study was a 2-arm parallel-group randomized controlled trial. The study was carried out on acute LBP patients who presented in the emergency department of the Istanbul Medipol University, at Esenler & Bagcilar in Istanbul in between October 2018 and October 2019. There were four physicians in the emergency department team and two of them were experienced chiropractors. Working hours were equally shared among these four physicians as shifts. The participants were allocated in one of the two groups: Medication-Only and Medication + Spinal Manipulation as the control group and the experimental group, respectively, in a simple random sampling order (Figure 1). The patients were assigned to experimental group and control group blindly by the registrar, depending on which physician was on duty when they were admitted to the emergency department. The observations were made before and after the treatment. Data were assessed immediately before the medication treatment, and 5 and 30 minutes after the treatment due to allowance for spinal manipulation and/or medication action timing, respectively. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional/regional/national ethics/committee/ethics board of the Istanbul Medipol University Ethics Committee (No: 441/2018) and informed consent was taken from all the patients. The trial protocol was published on ClinicalTrials.gov (NCT04110119). Trial conduct and reporting were in accordance with CONSORT statement (22).
Acute LBP was diagnosed according to the duration of LBP among patients that presented in the emergency department with LBP, where patients with <6 weeks of LBP were preliminarily diagnosed with acute LBP (4). Inclusion and exclusion criteria were determined in accordance with the WHO guidelines on basic training and safety in chiropractic (23). Inclusion criteria were being aged between 18 and 65, having acute LBP, persisting less than 6 weeks, meeting the diagnostic classification of 1 or 2 according to the Quebec Task Force on Spinal Disorders (23). Exclusion criteria were having medical history of anomalies such as dens hypoplasia, unstable os odontoideum, etc., acute fracture, spinal cord tumour, acute infection such as osteomyelitis, septic discitis, and tuberculosis of the spine, meningeal tumour, haematomas, malignancy of the spine, frank disc herniation with accompanying signs of progressive neurological deficit, dislocation of a vertebra, aggressive types of benign tumours, such as an aneurismal bone cyst, giant cell tumour, osteoblastoma or osteoid osteoma, internal fixation/stabilization devices, cauda equina syndrome, having previous spine surgery, spinal nerve root irritation or deficits, LBP due to occupational accidents, body mass index (BMI) >30, pregnancy, hypertension, psychotic disease (23). After the trial commenced there were not any changes to trial outcomes.
Intervention
Patients who presented in the ED with acute LBP and received the same pharmacological treatment were divided into two groups: The control group was the Medication-Only Group; participants were the patients with acute LBP who have undergone routine conventional pharmacological treatment consists of intramuscular injection of NSAID and myorelaxant combination in the ED. Experimental group was the Medication + Spinal Manipulation Group; participants were the patients with acute LBP who received spinal manipulation immediately after the same pharmacological treatment as in the control group in the emergency department. The pharmacological treatment consists of intramuscular injection of NSAID (diclophenac sodium 75 mg) and myorelaxant (thiocolchicoside 4 mg), administered only once.
The spinal manipulation treatment consists of high speed and low amplitude spinal thrust to lumbar spine of participants. It was applied only once. This session was to be delivered to each patient in 5 minutes just after the medication treatment. Spinal manipulation was performed by experienced chiropractor medical doctors who had an add-on training for that after their medical education. The patients did not have to pay any extra fee for the spinal manipulation treatment.
Both groups were treated by medical physicians under the supervision of specialists from the departments of Emergency Medicine, Physiotherapy, Physical Therapy & Rehabilitation Medicine.
Outcome assessment
Treatment response was measured at the individual level by a self-report of data using a face-to-face interviewer-administered the Visual Analog Scale (VAS) for pain which consists of a 10 cm straight line with the endpoints defining extreme limits such as ‘no pain’ and the ‘worst pain’ (24). The patient was asked to mark his pain level on the line between the two endpoints. The distance between ‘no pain’ and the mark showed the patient’s pain.
Statistical analysis
Descriptive statistics were presented as mean, standard deviation, median (minimum-maximum), frequency and percentage. The normality of data distribution was tested using the Kolmogorov-Smirnov test. The Mann-Whitney U-test and t-test were used for the analysis of independent quantitative variables (weight, height, BMI, VAS score) and Wilcoxon test was used for the analysis of dependent quantitative variables (VAS score changes in the group). The chi-square test was used for the analysis of independent qualitative variables (gender). Spearman’s correlation analysis was used for correlation analysis. Data were analyzed using IBM SPSS Statistics software v20.0 (IBM Corp., Armonk, NY, USA).
Results
A total of 152 patients were enrolled with acute LBP in the emergency department during that period. After the assessment for eligibility, 54 of them were excluded. Therefore, the study allocated a total of 98 patients (49 medication-only and 49 medication + spinal manipulation). All of the of participants completed the follow-up and included in the main analysis. The mean age of the subjects was 32.4, and 59 of the participants were male (60.2%). The mean BMI of the subjects was 26.4 (Table 1). The BMI distributions and initial VAS scores of the two groups were not significantly different. The intervention and comparison groups did not statistically differ with respect to demographic data such as gender, age, etc. (Table 2).
Table 1
| Variable | Min–Max | Median | Mean ± SD, n (%) |
|---|---|---|---|
| Age (years) | 16.0–57.0 | 32.0 | 32.4±8.5 |
| Weight (kg) | 55.0–96.0 | 76.5 | 77.2±10.2 |
| Height (m) | 1.5–1.9 | 1.7 | 1.7±0.1 |
| BMI | 19.5–29.8 | 26.5 | 26.4±2.4 |
| Pain VAS | |||
| Initial | 3.0–10.0 | 7.0 | 7.2±1.5 |
| 5th minute | 1.0–9.0 | 5.0 | 5.0±2.3 |
| 30th minute | 0.0–8.0 | 2.0 | 2.3±1.7 |
| Pain duration (hours) | 0.1–360.0 | 24.0 | 41.5±62.7 |
BMI, body mass index; VAS, Visual Analog Scale; SD, standard deviation.
Table 2
| Variable | Control group | Experimental group | Statistical methods | |||
|---|---|---|---|---|---|---|
| Mean ± SD, n (%) | Median | Mean ± SD, n (%) | Median | |||
| Age | 32.0±9.4 | 31.0 | 32.7±7.5 | 32.0 | t | |
| Gender | ||||||
| Female | 20 (40.8%) | 19 (38.8%) | X2 | |||
| Male | 29 (59.2%) | 30 (61.2%) | ||||
| Weight (kg) | 77.2±10.2 | 78.0 | 77.2±10.2 | 75.0 | m | |
| Height (m) | 1.7±0.1 | 1.7 | 1.7±0.1 | 1.7 | m | |
| BMI | 26.8±2.5 | 27.7 | 26.1±2.3 | 25.4 | m | |
t, independent sampling
No significant adverse events were observed with any of the patients. The 5th minute and 30th minute VAS scores were lower than initial VAS scores for both groups (P˂0.05 and P˂0.05, respectively). However, the decrease in VAS scores at 5th and 30th minute marks were significantly greater in the experimental group (P˂0.05) (Figure 2 and Table 3).
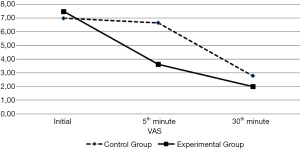
Table 3
| Variable | VAS score | P | Statistical methods | ||||
|---|---|---|---|---|---|---|---|
| Control group | Experimental group | ||||||
| Mean ± SD | Median | Mean ± SD | Median | ||||
| Initial | 6.9±1.6 | 7.0 | 7.4±1.5 | 8.0 | 0.130 | m | |
| 5th minute | 6.6±1.6 | 7.0 | 3.4±1.7 | 4.0 | 0.000 | m | |
| 30th minute | 2.7±1.9 | 2.0 | 1.9±1.3 | 2.0 | 0.041 | m | |
| Change in 5 minutes | 0.4±0.7 | 0.0 | 4.0±1.5 | 4.0 | 0.000 | m | |
| Change in the group | 0.001 | w | 0.000 | w | |||
| Change in 30 minutes | 4.2±1.5 | 5.0 | 5.5±1.6 | 6.0 | 0.000 | m | |
| Change in the group | 0.000 | w | 0.000 | w | |||
| Change in 5th to 30th minute | 3.86±1.39 | 4 | 1.51±1.063 | 2 | 0.000 | m | |
| Change in the group | 0.000 | w | 0.000 | w | |||
VAS, Visual Analog Scale; m, Mann-Whitney U test; w, Wilcoxon test; SD, standard deviation.
All of the patients were administered for observation, and then discharged after 30 minutes followed by being referred to physiotherapy department. Diagnostic imaging techniques or any other relevant investigation were not used.
Discussion
In our study, we compared the short-term outcomes of spinal manipulation + pharmacological care against only- pharmacological care in acute LBP patients in the emergency department and the results showed that integrative spinal manipulation was effective in the short-term treatment of acute LBP patients and no important adverse events were reported with any of the participants.
Multiple studies have been conducted on how the spinal manipulation works biomechanically and neurologically from the connective tissue and peripheral nerves to the central nervous system both at the cord level and higher cortical regions, however the exact mechanisms involved are not well understood (25).
Our findings are consistent with the systematic reviews concerning the effectiveness of spinal manipulation (24,25). In our study, there were no serious adverse events with any type of treatment. That can be because of the exclusion of elderly people with the risk of having serious causes of LBP that may contra-indicate use of spinal manipulation, e.g., metastatic disease, or primary malignancy, infection, etc.
There are several studies that support the safety and effectiveness of spinal manipulation for LBP (25,26). However, some authors conclude that spinal manipulation is not associated with statistically significant benefits compared to other interventions (11). On the other hand, some authors point out to the benefits of spinal manipulation to a certain extent (27,28), whereas others do not recommend it for acute LBP (29).
There is moderate evidence that shows spinal manipulation can be as equally effective for LBP as physical therapy. Despite the lack of conclusive evidence, some of the available studies point to the comparable outcomes of spinal manipulation, exercise therapy, and medical care (30). According to a recent systematic review and meta-analysis, spinal manipulation by experienced chiropractors can provide comparable results to NSAIDs for LBP without any significant damage (31). However, the large heterogeneity of available studies makes it difficult to reach a definitive conclusion (25,28).
LBP is a medical problem that is dealt daily in the primary care and emergency department. Emergency care is an integral part of general practice, and primary care physicians play an essential role in the management of emergencies; therefore, spinal manipulation can be more widely applied in the emergency or primary treatment of acute LBP in the context of integrative medicine.
Since LBP is associated with many risk factors, a detailed examination and medical history are required to determine the safety of spinal manipulation. Chiropractors are often the first contact for patients with LBP thus these patients require detailed medical history together with a thorough examination and other assessment including imaging when indicated to determine any significant undiagnosed health conditions.
This study has the limitations of observing the efficacy of “addition” of manipulation, but not the manipulation alone. Furthermore, due to the application of spinal manipulation in the study, blindness could not be done. Moreover, just the short-term effectiveness of integrative spinal manipulation was investigated; therefore, the long-term effectiveness is not known. Besides that, it was just on acute LBP, and therefore not covering the chronic LBP conditions. Results can’t be generalized. In order to generalize the results, it should be considered to study with larger populations.
Conclusions
Integrative spinal manipulation as an add-on treatment to medication in the patients with acute-LBP significantly reduced VAS scores compared to standard treatment. We did not detect any significant safety concerns. The integration of spinal manipulation may improve the short-term outcomes for medication-treated LBP patients presenting to emergency department.
To the best of our knowledge, this is the first study to investigate the efficacy of additional spinal manipulation in patients with acute LBP in the emergency department. Our findings can contribute to the consideration of spinal manipulation as an integrative treatment option for acute-LBP in general practice. It is suggested that both primary healthcare and emergency medicine professionals should consider spinal manipulation for patients with acute-LBP in the context of integrative medicine. Further randomised comparative studies are required to determine the long-term effectiveness of integrative management strategies for LBP.
Acknowledgments
The authors are grateful to all the patients that participated in the study. We wish to thank to all the staff at the Emergency Department of the Istanbul Medipol University, with special appreciation to Hilal Tuylu.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://dx.doi.org/10.21037/lcm-21-11
Data Sharing Statement: Available at https://dx.doi.org/10.21037/lcm-21-11
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/lcm-21-11). ATA reports that he is from Scientific Office, U-merge Ltd. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study design was approved by the Istanbul Medipol University Ethics Committee (No: 441/2018). Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hincapié CA, Tomlinson GA, Côté P, et al. Chiropractic care and risk for acute lumbar disc herniation: a population-based self-controlled case series study. Eur Spine J 2018;27:1526-37. [Crossref] [PubMed]
- Priority Medicines for Europe and the World (WHO) [Internet]. Vol. 2020. World Health Organization; 2013. Available online: https://www.who.int/medicines/areas/priority_medicines/Ch6_24LBP.pdf
- Manchikanti L, Singh V, Falco FJ, et al. Epidemiology of low back pain in adults. Neuromodulation 2014;17:3-10. [Crossref] [PubMed]
- Koes BW, van Tulder M, Lin CW, et al. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 2010;19:2075-94. [Crossref] [PubMed]
- Bussières AE, Stewart G, Al-Zoubi F, et al. Spinal Manipulative Therapy and Other Conservative Treatments for Low Back Pain: A Guideline From the Canadian Chiropractic Guideline Initiative. J Manipulative Physiol Ther 2018;41:265-93. [Crossref] [PubMed]
- Patel HD, Uppin RB, Naidu AR, et al. Efficacy and Safety of Combination of NSAIDs and Muscle Relaxants in the Management of Acute Low Back Pain. Pain Ther 2019;8:121-32. [Crossref] [PubMed]
- Galliker G, Scherer DE, Trippolini MA, et al. Low Back Pain in the Emergency Department: Prevalence of Serious Spinal Pathologies and Diagnostic Accuracy of Red Flags. Am J Med 2020;133:60-72.e14. [Crossref] [PubMed]
- Edwards J, Hayden J, Asbridge M, et al. Prevalence of low back pain in emergency settings: a systematic review and meta-analysis. BMC Musculoskelet Disord 2017;18:143. [Crossref] [PubMed]
- Brody AM, Murphy E, Flack JM, et al. Primary care in the emergency department -- an untapped resource for public health research and innovation. West Indian Med J 2014;63:234-7. [PubMed]
- Carter GT, Duong V, Ho S, et al. Side effects of commonly prescribed analgesic medications. Phys Med Rehabil Clin N Am 2014;25:457-70. [Crossref] [PubMed]
- Rubinstein SM, Terwee CB, Assendelft WJ, et al. Spinal manipulative therapy for acute low-back pain. Cochrane Database Syst Rev 2012;CD008880 [Crossref] [PubMed]
- Foster NE, Bishop A, Thomas E, et al. Illness perceptions of low back pain patients in primary care: what are they, do they change and are they associated with outcome? Pain 2008;136:177-87. [Crossref] [PubMed]
- Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet 2018;391:2368-83. [Crossref] [PubMed]
- Çağlayan HZB, Ataoğlu EE, Kibaroğlu S. The assessment of efficiency of traditional and complementary medicine practices in neurology. Turk Noroloji Dergisi 2018;24:111-6. [Crossref]
- Ağaoğlu MH, Salık E, Mangan GM, et al. The Place and Importance of Chiropractic Science that Got Started on “‘Innate Intelligence’” Philosophy of D.D. Palmer in the World and in Turkey. Journal of Traditional Medical Complementary Therapies 2018;1:93-8. [Crossref]
- McClelland G. The American Chiropractic Association and primary care. J Chiropr Med 2002;1:180-3. [Crossref] [PubMed]
- Pereira MG, Roios E, Pereira M. Functional disability in patients with low back pain: the mediator role of suffering and beliefs about pain control in patients receiving physical and chiropractic treatment. Braz J Phys Ther 2017;21:465-72. [Crossref] [PubMed]
- Eklund A, Jensen I, Lohela-Karlsson M, et al. The Nordic Maintenance Care program: Effectiveness of chiropractic maintenance care versus symptom-guided treatment for recurrent and persistent low back pain-A pragmatic randomized controlled trial. PLoS One 2018;13:e0203029 [Crossref] [PubMed]
- Bronfort G, Haas M, Evans R, et al. Evidence-informed management of chronic low back pain with spinal manipulation and mobilization. Spine J 2008;8:213-25. [Crossref] [PubMed]
- Sixty-Seventh World Health Assembly WHA67.18 Traditional medicine (WHO) [Internet]. Vol. 2020. World Health Organization; 2014. Available online: https://apps.who.int/gb/ebwha/pdf_files/WHA67/A67_R18-en.pdf?ua=1
- Geleneksel ve Tamamlayıcı Tıp Uygulamaları Yonetmeligi [Internet]. Vol. 2020. Resmi Gazete; 2019. Available online: http://www.resmigazete.gov.tr/eskiler/2014/10/20141027-3.htm
- Schulz KF, Altman DG, Moher D, et al. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [Crossref] [PubMed]
- World Health Organization. WHO guidelines on basic training and safety in chiropractic [Internet]. 2005 [cited 2021 Jun 20]. Available online: https://apps.who.int/iris/handle/10665/43352
- Chiarotto A, Maxwell LJ, Ostelo RW, et al. Measurement Properties of Visual Analogue Scale, Numeric Rating Scale, and Pain Severity Subscale of the Brief Pain Inventory in Patients With Low Back Pain: A Systematic Review. J Pain 2019;20:245-63. [Crossref] [PubMed]
- Paige NM, Miake-Lye IM, Booth MS, et al. Association of Spinal Manipulative Therapy With Clinical Benefit and Harm for Acute Low Back Pain: Systematic Review and Meta-analysis. JAMA 2017;317:1451-60. [Crossref] [PubMed]
- Walker BF, French SD, Grant W, et al. Combined chiropractic interventions for low-back pain. Cochrane Database Syst Rev 2010;CD005427 [PubMed]
- Ruddock JK, Sallis H, Ness A, et al. Spinal Manipulation Vs Sham Manipulation for Nonspecific Low Back Pain: A Systematic Review and Meta-analysis. J Chiropr Med 2016;15:165-83. [Crossref] [PubMed]
- Shekelle PG, Paige NM, Miake-Lye IM, et al. The Effectiveness and Harms of Spinal Manipulative Therapy for the Treatment of Acute Neck and Lower Back Pain: A Systematic Review [Internet]. Washington (DC): Department of Veterans Affairs (US); 2017 Apr.
- Rothberg S, Friedman BW. Complementary therapies in addition to medication for patients with nonchronic, nonradicular low back pain: a systematic review. Am J Emerg Med 2017;35:55-61. [Crossref] [PubMed]
- Blanchette MA, Stochkendahl MJ, Borges Da Silva R, et al. Effectiveness and Economic Evaluation of Chiropractic Care for the Treatment of Low Back Pain: A Systematic Review of Pragmatic Studies. PLoS One 2016;11:e0160037 [Crossref] [PubMed]
- Whedon JM, Toler AWJ, Goehl JM, et al. Association Between Utilization of Chiropractic Services for Treatment of Low Back Pain and Risk of Adverse Drug Events. J Manipulative Physiol Ther 2018;41:383-8. [Crossref] [PubMed]
Cite this article as: Atayoglu AT, Korhan S, Temizkan E, Emenli MB, Koc H, Ucar D, Atac A, Turan M, Guner M. Short-term efficacy of spinal manipulation in addition to pharmacological treatment of acute low back pain in the emergency department: a randomized controlled trial. Longhua Chin Med 2021;4:22.