
From traditional Mediterranean, Ayurvedic and Chinese medicine to the modern time: integration of pathophysiological, medical and epistemological knowledge
Introduction: aim and methods
In this work we present a narrative overview as an educational article presenting a broad perspective about modern integrative medicine approach, describing its historical premises, and philosophical development. Our aim, discussing integrative medicine theory and context, is to provoke thought and controversy hopefully presenting epistemological perspectives in a balanced manner, stimulating scholarly dialog amongst readers. We do not present a systematic review of the literature on a specific topic, but we would like to inform the reader about different thought patterns that can guide scientific research and medical treatment.
We referred to our personal experience, electronic databases (PUBMED, Cochrane Database of Systematic Reviews) and authoritative texts (reported in the references section) for the last part of the text dealing with modern biomedical and biochemical studies about integrative medicine. Moreover, in the first historical section, we referred to our personal experience and our research conducted so far reading and translating directly from the Sanskrit, Greek and Latin the ancient medical text indicated in the bibliography, along with Authoritative commentaries made on them.
Traditional medicine
Greek classic medicine
Greek classic medicine developed from the 5th century before current era (BCE) to the 2nd century CE in a wide variety of geographic and cultural contexts, ranging from Greek continent and colonies in the islands and coasts of the Mediterranean Sea, to Hellenistic kingdoms and the Roman Empire. This broad range of time, places, and varieties of socio-cultural contexts reflect an extremely rich and complex scientific scenario. Indeed, Greek medicine saw the development of three main medical schools, namely the Hippocratic, the Alexandrian and the Galenic one, and a variety of minor ones. Those schools were represented by physicians, who supported different ideas and approaches, sometimes scarcely reconcilable even within the same school.
The Hippocratic School developed during the 5th and 4th cent. BC in the Greek island of Cos in the Aegean Sea, close to the coast of current Turkey. According to the tradition, it was founded by Hippocrates (c. 460-377 BCE), a historical figure, who gradually acquired a mythic aura (1-4). To Hippocrates is traditionally attributed a corpus of about 60 texts which, however, are very diverse in style and subject, making the authorship dubious. Indeed, opinions expressed in those texts are so contradictory that it is unlikely for the corpus to represent the work of a single medical writer (3,5). Most texts are exploratory arguments, debating with and criticizing other authors. A sophisticated reasoning is used to understand the mechanisms underlying diseases and to categorize collections of clinical symptoms (2). Merit of the Hippocratic School was to replace the “ontological” concept, where diseases were external “supernatural” entities send by gods, with a new vision of diseases, as caused by internal factors altering the equilibrium of the body by perturbing its physiology (6). Internal disorders could be caused also by external “natural” factors, such as the atmospheric conditions, the quality of water, food, air or habits of individuals (included their psychic attitudes) and populations. Hippocrates and his followers were inspired by pre-Socratic philosophy, which based its knowledge on observation and rational thinking for explaining natural phenomena. A cross-fertilization between philosophy and medicine was particularly evident at the beginning of the 5th century, represented by paradigmatic figures such as Pythagoras (c. 570-490 BCE) and his disciple Alcmaeon of Croton (5th cent. BCE). In the late 5th centuries there were other important philosopher-physicians such as Empedocles (c. 490-430 BCE), Diogenes of Apollonia (born c. 460 BCE) and Democritus of Abdera (born c. 460 BCE) (1,2). Empedocles developed the theory of the four elements—air, water, earth and fire—whose different proportional relationship explained the differences between substances. Concurrent with this notion, he also tried to explain human physiology (7). The theory of four elements, combined with the theory of four qualities (hot, cold, dry and wet), became a fundamental theoretical model for the humoral conceptions, which was one of the most important achievements of Hippocratic medicine.
In many important books of the Hippocratic Corpus, such as the Epidemics, Prognostics, Regimen in Acute Diseases, Affections, clinical diagnosis and prognosis were two strictly connected moments. The Hippocratic authors tried to find some “regularity” in the great variability of symptoms, course of diseases, patients’ habits, geographic and climatic characteristics of towns and countries, seasons, and so on. They tried to connect all these features using detailed and systematic observations, creating “clinical entities” which, even if often not ascribable to our current nosology, were used as models for many following generations of Western physicians. The principal “physiological” and “patho-physiological” model developed by Hippocratic medicine was that of the humors, which inspired Western medicine for centuries and represents another fundamental achievement of that school. In many books of the Hippocratic Corpus, the body was viewed as a system of conduits (which should not be identified anatomically solely as nerves or blood vessels, not yet clearly identified at that time, but also as “functional metabolic pathways” according to a modern terminology) where factors of diseases could “circulate”. Among them, the “humors” played a leading role. Disorders developed when one or more humors were peccant, morbific, accumulated in some parts or deficient in others. While different kind of “humors” were mentioned in the Hippocratic Corpus, only in the work On the Nature of Man a systematic theory was established for the first time. Briefly, health and disease of a man were connected to the reciprocal balance or unbalance, respectively, between four precise humors, namely blood, phlegm, black and yellow bile. Diseases arose when the mixture of humors became unbalanced, or when one humor became isolated (2). It is important to highlight that in the Nature of Man the theory of the four humors is not connected to the four elements of the universe (air, fire, water, earth), and there is no trace of its development into a theory of the four temperaments or of their corresponding character types (1). Only later, and particularly in the work of Galen, the humors were connected with the Empedocles’ theory of elements and qualities. Blood corresponded to air, and it was warm and humid; phlegm correlated with water, and was cold and humid; black bile, connected with earth, was cold and dry; and, finally, yellow bile, associated with fire, was hot and dry.
The Hippocratic authors never directly addressed the question whether they could, or should, practice dissection on human beings (1). Of course, a certain anatomical knowledge is evidenced throughout the Hippocratic Corpus, but human anatomy, per se, was not practiced. The first medical school in which human anatomy was systematically investigated thought dissection flourished in Alexandria of Egypt under the Ptolemaic dynasty, in particular in the first fifty years of the 3rd century BC. The main school representatives were Herophilus of Chalcedon (c. 330-250 BCE) and Erasistratus of Ceos (c. 330-250 BCE) (8-10). The Hippocratic medicine was an “art” almost exclusively centered on clinical problems and the body was viewed as a sort of “black box” in which the humoral patho-physiology was deduced almost exclusively from the observation of input and output materials (11). Herophilus and Erasistratus revolutionized this model by opening the “black box”, i.e., dissecting the human body to understand first the normal physiology and afterwards the patho-physiological processes. Thanks to them an unprecedented knowledge of the vascular and nervous systems, as well as of the brain, heart, and liver was achieved. Herophilus distinguished between motor and sensory nerves. The sensory nerves were filled with pneuma, which transmitted sensation from the sensitive organs to the brain. The pneuma was the result of the inspired air, which was inhaled by the dilatation of lungs and thorax, acting as bellows. The brain was the source of nerves and the unique responsible for all sense and motion. He also distinguished arteries from veins, although he did not fully understand their functions (8,10). He believed that veins derived from the liver and contained the blood which nourished all the parts of the body. Arteries, instead, contained pneuma and probably also some blood for nourishing arteries tunicae (10). The presence of two pneuma, one inside the nerves and another in the arteries, anticipated the distinction between psychic and vital pneuma, which would become canonic in the later tradition (10,11). Erasistratus based his model upon a corpuscular theory. According to this theory, matter consisted of tiny particles interspersed with void. The nutritive particles of the blood were absorbed by the tissues through fine pores in the walls of the capillary veins. This absorption was due to a process of filling the empty spaces formed by the degradation of matter produced in the body by its living activity (12), according to the notion that vacuum tended to fill itself from neighboring matter (13). With regard to the arterial system, Erasistratus believed that it was filled with pneuma, which was the product of the process of inhalation of air. The pneuma arrived from the lungs to the left ventricle of the heart, which attracted during its diastole. Through the arterial system, the pneuma arrived at the muscles, forming the energetic principles of muscular movements: it became, then, the “vital pneuma”. A part of it arrived at brain ventricles, where it was furtherly transformed into “psychic pneuma”, responsible of sensations, voluntary actions and intelligence (11). In Erasistratus’ physiology, there were three principal systems: the venous, filled with blood, the arterial, filled with vital pneuma, and the nervous system, filled with psychic pneuma. These systems had no visible communications. So, for explaining how the blood could nourish the arteries and how sensations could arrive where there were no visible nerves, Erasistratus proposed the existence of an invisible system of veins, arteries and nerves, called triplokia, supporting the reciprocal and physiological communication between the visible and the invisible structures (14). On the base of this model, Erasistratus derived also a new pathology. Disease were caused by a form of “plethora”, that is, an excess of blood which overflowed into either the arterial or the nervous system. If the blood overflowed into the arteries, inflammatory and febrile diseases arose. If it overflowed into the nerves, different kind of “paralysis” developed. Therapy followed this model by reducing the overflowing of blood by means of diets, purges or emetics. Galen of Pergamon (c. 129-216 CE) was a Greek Roman physician who is considered, with Hippocrates, the father of Western medicine (15). Galen was able to reconcile, in an eclectic way, the Hippocratic and the Alexandrian traditions. He integrated the clinical and the anatomo-physiological approaches adding important notions and inspirations from Plato, Aristotle and the Stoics (16). Galen furtherly developed the “Hippocratic” system of humors and incorporated into it the theory of pneuma from the Alexandrian school. He modified the previous concepts by anatomical investigations and vivisections on animals, thus elaborating a new physiological model. In his On the Complexions, in particular, he stated that bodies were a mixture of the primary qualities (hot, cold, dry and wet), or better, of their correlated elements, namely air, fire, water and earth (17). In the On the Natural Faculties, he further connected to the qualities and to the elements the four humors and establishing four basic “temperaments” (18). In the On the Usefulness of the Parts and On the Affected Parts, instead, Galen treated the “homogeneous” and “heterogeneous” parts of the “human” body. All these works, described the anatomy, physiology, and a sort of anatomically oriented pathology of men. Galen recovered and developed an “archaic” concept, namely that of “eucrasia” (19). The body was in a healthy state if there was a “good mixture” of elements and a good proportion between its anatomical parts, while it became ill if there was a “dyscrasia” (literally meaning “unbalance” and indicating, in “modern” terms, a pathologic alteration of the chemical, chemico-physical, immunological characteristics of organic liquids and blood). In his On the Therapeutic Method and On Temperaments, Galen distinguished eight basic kind of “dyscrasia”: in four a single quality was dominant and in the remaining four two qualities prevailed. This model influenced also the therapy, as drugs were created according to the elements and qualities of their compounds and in correlation with the particular patient dyscrasia (20). Moreover, Galen further developed the link between humors and age. Galen connected the four humors and the four stages of life in a system including humors, seasons and ages: blood- spring-infancy; yellow bile-summer and youth; black bile-autumn and maturity; phlegm-winter and older age. He used this new correspondence to create an original relationship between the elements, the humors and character.
Chinese traditional medicine
As in Indian and Greek history, at a certain point, medicine started to be strictly connected with “natural philosophy”, i.e., with the knowledge of the fundamental elements and mechanism of the natural world. In Chinese history this happened, in particular, during the Hang Dynasty (206 BC-220 CE). The most classic Chinese medical text, The Yellow Emperor’s Inner Canon of Medicine stated that: Although the origins of illnesses are traceable to many causes, all of them result from (something) evil. […] That is to say, everything that is not part of the normal order in the human organism, (such as) wind, cold, dampness, hunger, fullness, taxation, and idleness, is evil - and not solely the influences of demons and epidemic illnesses (as some authors have claimed) (21).
With the consolidation of “Imperial Unity”, three concepts were finally codified, becoming the core of Chinese medicine: Qi, Yin-Yang and Wu Xing. The qi approximately refers to the energetic feature of the cosmos and the human body, even if, at the same time, indicates a material entity, or, rather, a sort of “psycho-physical matter” ubiquitous in the universe, and characterized according to different degrees of “thickening”. For instance, a stone represents an object with a deeply thickened qi, while mind and spirit represent states of qi particularly rarefied. “Sky” (or “Heaven”) and “Earth” symbolize the two most extreme opposites, where the first is composed of the maximum rarefaction and dispersion of qi, while the second is composed of its maximum condensation and aggregation. Several scholars noted the affinity between the oriental qi concept and the Western concept of energy (22,23). Yin-Yang represents the bipolar aspect of any phenomenon of the reality, both spatial and temporal, which is characterized by the presence of opposites, but complementary aspects. The concept of Yin-Yang derives from the ideas of yi (mutation), pien (cyclic change) and t’ong (mutual permeation) (24). As resumed by Francisco Lozano:
Yin is associated to qualities such as cold, rest, responsiveness, passivity, darkness, structure, the interior, downward and inward motion, and decrease. By contrast, yang is associated with heat, stimulation, movement, activity, light, the exterior, upward and outward motion, and increase. It is important to observe that these aspects occur only in relation to each other (i.e., cold can be defined only by the knowledge of heat, darkness by the presence or absence of light, and so on). In medicine, yinyang theory would be applied to opposites such as structure (yin) and function (yang), the lower body (yin) in relation to the upper body (yang); however, the concepts of yinyang are never absolute. They are applied to given objects in order to express their relation to other objects, actions, or processes (25).
Finally, Wu Xing, also named “Five Phases” theory, refers to the five “elements”—Fire, Earth, Metal, Water, and Wood—which constituted the essential principles of natural world. The term “element” could be misleading: it should be preferable to translate this concept as “movement” (26,27) or “phase” (28). These components of the reality, in fact, are better understood as five “phases” of cycles of transformation and interrelation. In particular, among them there are connections of “generation” (sheng cycle), relationships of “control” or “overact” (ke cycle), and “insult” (wu cycle) (29). These cycles, in turn, are ruled by the pivotal dynamic of Yin-Yang. These phases, in their immutable cycle of succession, were correlated with cardinal directions, seasons, colors, musical tones, and bodily organs. In connection with the internal tissues, organs and structures associated, they are also fundamental in acupuncture techniques.
An important distinction in Chinese Traditional Medicine is between viscera zang (Yang) and organs fu (Yin). Viscera zang transform and digest, eliminating impure residuals from solid foods and liquids. The organs fu collect pure essences resulted from the transformation processes realized by viscera zang. These pure essences, created by zang and accumulated by fu, are essentially characterized by the qi, which represents the vital force needed by all the body’s parts for living. The zangs store but do not eliminate, while the fu eliminate but do not store. What the organs stored was described in the The Yellow Emperor’s Inner Canon of Medicine as, ‘we read that the liver stores the blood, which contains the soul; that the heart stores the pulse, which contains the spirit; that the spleen stores nutrition, which contains the thoughts; that the lungs store the breath, which contains energy, and finally, that the kidneys store the germinating principle, which contains the will’ (30).
Viscera zang are six: stomach, small intestine, large intestine, urinary bladder, gallbladder, and the so called “triple burner”. Organs fu are five: kidneys, liver, heart (xin), spleen, and lungs.
The five elements, as already stated, are principles of transformation strictly related with seasonal cycles. Health derives from conforming to the activities and characteristics typical of each season, in relationship with the season immediately preceding and the following one, in correlation with all the features analogically connected with each one of the given element, included bodily organs. In the Canon, for instance, we find the following statement:
The three months of springtime are called period of beginning and development (of life). […] During this period (the body) should be encouraged to living and not to dying; (to it) should be freely given and not deprive it from something; it should be rewarded and not punished. […] Those who disobey to the springtime laws will be punished with a liver disease. To them, the following summer will brought shivers and changing (in worst); therefore they will have very little to support their development (during the summer) (31).
Acupuncture is still one of the best known and diffused practices of traditional Chinese medicine, even if it is still debated in culturally Western countries (32-34). The Chinese name of that practice is Zhenjiu, meaning needle and moxa, while “acupuncture” comes from the Latin words acu (needle) and puncture (34). Probably, the earliest written mention of the practice of acupuncture can be traced in a manuscript found in a tomb of the early Han period: “[…] When the qi rises at one moment and falls in the next, pierce it with a stone lancet at the back of the knee and the elbow” (35). Acupuncture emerged in its complete or “orthodox” form during the Han Dynasty, as a product of the Yin-Yang and Five Phases theories (35). This practice consists in the introduction of hot or cold needles into the body at certain specific points. These points were crucial sites of the “channels” or “meridians” (named mo) where the qi flowed around the body. They were placed, in particular, where the channels crossed and around the joints (35). The needles could be made of flint, bone, silver, gold, copper, brass or steel, according to different periods, uses, or scopes. For the same reason, they could be of several dimensions (in width and length). Again, in the Canon, 365 points are described to correspond with the days in the year, but they could vary with different authors, arriving up to more than 600 points. The theory on which acupuncture was based stated that the body was crossed by a system of meridians through which the life-energy known as qi flowed. There were 12 principal “meridians”, divided into Yin and Yang sets and grouped according to their belonging to the arms or legs sections. Five-Shu points, next to the nails, form the origin of the 12 Yin and Yang meridians and are correlated with the five elements. They are particularly important in acupuncture practice (36). These points, in fact, are on the major surface of the body on the fingers and toes, and gradually enter within the body all along the course of the channels. For that reasons, the points on these extremities are particularly susceptible to external pathological factors (i.e., wind, cold and humidity) and consequently are of major importance for therapy (29). They are named according to distance from the fingers or toes and the elbow or knees, respectively. The first, on the surface of fingers and toes, is named well (jĭng), the second source (ying), the third brook (shu), the fourth river (jīng) and the fifth sea (he) (29). Their names are based on the analogy between these channels and the nature, where a well could gradually become a river and flows into the sea. Through this circuit, the qi moved around the body and health required that the circuit was aligned with cosmic movements. To be “weak”, move in the wrong direction, or be blocked or stagnant inside any part of the body means disease (37).
This extremely complex set of theories, principles, ideas and practices presents some common basic characteristics which can be summarized as follows. First, the strict relationship and cross-fertilization between philosophy and medicine guided both classic Greek and ancient Chinese physicians in their understanding of the human body as an entity strictly connected with nature and their fundamental elements. The four or five elements were principles regulating both natural phenomena and the physiology of human being. The balance or unbalance of these elements - in their strict relationship with the four humors and pneuma of the body, for the Greek Medicine, and the system of Qi for the Chinese tradition—determined health and disease. Therefore, the body was seen as an integrated system and its health and disease were correlated to the balance or unbalance of its entire component, both anatomical and psychological. Moreover, the body was an integrated entity with nature. Microcosm and macrocosm were strictly interconnected, so that environmental factors played a major role in determining health and disease. That health and disease were commonly conceived as a state of balance or unbalance between mind and body, namely pneuma or qi and the elements or humors, means that, in classic Greek and Chinese medicines, the conception that health and disease could be standardized states did not exist. In other words, any individual was a unique product of the interaction between the basic psychic and physical elements that, in turn, was determined by his specific development, habit and interaction with the environment. The bodily and natural principles were categorized not only in a quantitative way, but also according to their qualities and they were viewed always in their interaction with the whole microcosm-macrocosm system.
Ayurvedic medicine
Āyurveda, the “science” (veda) of “(long) life” (āyus), is the earliest form of rational medicine of India1 and one of the few pre-modern medical traditions which continues to be practiced. Āyurvedic literature, redacted in Sanskrit, consists of compendia (saṃhitā), glosses (variously called bhāṣya, dīpikā, prakāśa, ṭippaṇī) and digests of materia medica (nighaṇṭu). The first medical compendia can be dated to the second half of the first millennium BCE, although they have been rewritten and expanded at multiple times across the centuries. By the 19th century, Indian scholars arranged the chief saṃhitās in two groups:
- The bṛhattrayī, or “greater triad”, comprising the Carakasaṃhitā (or Agniveśatantra) (1st–2nd century) (38), the Suśrutasaṃhitā (3rd–4th century)2 (39) and the Aṣṭāṅgahṛdayasaṃhitā of Vāgbhaṭa (6th–7th centuries)3 (40,41);
- The laghutrayī, or “lesser triad”, made of the Mādhavanidāna of Mādhavakara (8th century) (42), the Śārṅgadharasaṃhitā (c. 14th century) (43) and the Bhāvaprakāśa of Bhāvamiśra (16th century) (44)4.
Āyurveda primarily aims at identifying the causes (hetu) and the symptoms (liṅga) of diseases (roga, vyādhi) as well as the remedies (auṣadha, lit. “herbs”) to ensure recovery, adequate quality of life and life expectancy. Although there is general agreement on the scope of medicine, views on pathology, diagnostics and therapeutics may vary to a great deal, thus making it hard to identify a standard. For the purpose of this article, the analysis will be limited to those medical theories, which examine health seekers as integrated within their social and environmental space.
According to a view first attested in the original work of Agniveśa (CaS i.1.54; cf. ii.1.3), the physician (vaidya) should try and understand pathological causes by considering the wrong (mithyāyoga), absent (ayoga) or excessive (atiyoga) association of the patient with time (kāla), intellect (buddhi)5 and sense organs (indriya)6.
The conceptualization of the human body and its formation provides the basis for holistic therapeutic approaches. Already in Caraka, we see that the embryo (garbha) is made of mother (mātṛ = blood), father (pitṛ = semen), the self (ātman), wholesomeness (sātmya), the juices (rasa) produced by the mother’s digestion and mental faculty (sattva) (CaS iii.3.3)7. Following gastric “cooking” (pācana, dīpana), food and beverages are transformed into the “three foundations” (tristhūṇa) of the body, namely (I) the seven tissues (saptadhātu), (II) the three humors (tridoṣa), i.e., wind (vāta), bile or choler (pitta) and phlegm (kapha or śleṣman), and (III) excreta (mala). (SuS i.14.10-12; cf. ŚāS i.5.11-12).
Since everything derives from food, which in turn results from aggregates (yukta) of the modifications (vikāra) of the five principal elements8, Āyurveda insists on the importance of the way in which a patient and environment relate to each other. Depending on the circumstances of the patient, environmental modifications can be avoided, if dangerous, sought for, if beneficial, or maintained, if appropriate.
Diseases are usually classified as internally caused (nija), invasive (āgantu) and mental (mānasa/mānasika) (CaS i.11, cf. SuS i.1, AHS i.1, BhāPr i.6.2). An alternative frame is provided by Suśruta, who identifies seven kinds of ailments: (I) ādibalapravṛtta, resulting from procreation, i.e., hereditary disorders; (II) janmabalapravṛtta: congenital diseases; (III) doṣabalapravṛtta: conditions resulting by aggravation or imbalance of the humors; (IV) saṃghātabalapravṛtta: disease caused by trauma and/or injuries; (V) kālabalapravṛtta: diseases resulting from atmospheric conditions; (VI) daivabalapravṛtta: diseases caused by the gods; (VII) svabhāvabalapravṛtta: conditions depending on natural factors (e.g., old age, hunger, thirst, etc.) (SuS i.24) (48). On each case, etiology is different. For instance, internal (i.e., physical) ailments can be imputed to the blockage of channels, the withholding of basic urges or problems regarding the seven tissues or the three humors. Conversely, invasive diseases may result from factors unrelated to the willing and lifestyle of the patient, e.g., wars, natural disasters, famines, failing policies and bad administration (leading to impoverishment, etc.), and, ultimately, disregarding the appropriate code of conduct (dharma). In the case of mental disorders, medical compendia signal as potential causes internal pathologies or external agents (e.g., “demonic” possession, misbehavior, etc.). It so emerges that, unlike what is found in far too many secondary sources, Āyurveda is not just “humoral” medicine, and certainly the “imbalance” of the doṣas is not the only cause of disease. Also, there is a discrepancy between the earliest tradition and slightly later sources.
Caraka and Buddhist sources call “dhātu” not just the seven bodily constituents but also the three humors. Only when the latter are found in the wrong part of the body9 or are aggravated (prakupita), they are called doṣas (lit. “defects”, “faults”, “vices”) and become pathogenic elements (doṣasaṃgraha, CaS i.1.57). Conversely, from Suśruta onwards, bile, wind and phlegm are always called doṣa. Further to that, it should be noted that whereas Caraka refers to tridoṣa (“three faults”), Suśruta says that physical diseases result from the ingestion of foods and beverages which causes the “imbalance” (vaiṣamya) of vāta, pitta, kapha and śoṇita (blood) or their “combination” (saṃnipāta) (SuS i.1.25b, cf. BheS i.26.34, ŚāS i.5.54) (49-51). This suggests that early Āyurveda was a somehow heterogeneous tradition with medical schools following different philosophical systems and having varied approaches to pathology and therapeutics. Only from around the 7th century, with the Aṣṭāṅgahṛdayasaṃhitā and the Aṣṭāṅgasaṃgraha of Vāgbhaṭa, if we agree on single authorship (52), a clear effort at systematization is discernible.
Since its early stages, Āyurveda indicates three therapeutic courses: the first is about the gods (daivavyapāśraya) (e.g., ritual offerings, prayers, austerities, repetition of mantras, etc.), the second requires reasoning (yuktivyapāśraya) and the third is about the control of the mind (sattvāvajaya), i.e., mental health (CaS i.11.54). More generally, treatment could be ritual (CaS i.30.21) or non-ritual. The latter is further divided into three approaches: without medicines, with medicines and surgical. Treatment without medicine is of great interest in that it demonstrates a profound awareness of the relation between patients, the environment in which they live as well as their own history and personal circumstances. As Caraka points out:
He [the wise person] should also make every effort to cultivate a knowledge of self, environment, family background, time, strength, and vigor (ātmadeśakulakālabalaśaktijñāna). And he should cultivate people who know about such matters. (CaS i.11.46).
Therapy without medicines includes, amongst the others, “pointing out dangers to the patient, or in surprising, making forget, agitate, delight, threaten, or strike him or her, or putting them to sleep” (53). Other important approaches concern not suppressing natural urges (navegāndhāraṇa) and planning appropriate regimens (ācāra). In the former case, which is detailed as early as Caraka, withholding urine, feces, semen, wind but also sneezing, clearing the throat, yawning, hunger, thirst, tears, sleep, or the “panting induced by exertion” (CaS i.7.3-4) are explained as the cause of several diseases. Yet to avoid excessive indulgence in satisfying impulses, the āyurvedic vaidya warns his patient to always keep in mind the importance of decorum and never favor ill will, bad taste and rudeness.
The concept of ācāra is equally important. Vāgbhaṭa’s Aṣṭāṅgahṛdayasaṃhitā, a text which provides the most effective synthesis of Indian medicine (54), discusses daily and seasonal regimen by examining environment (cara) and body (deha) in relation to time (kāla) and land (deśa) (cf. BhāPr i.5). This led Zimmerman to theorize that “Āyurveda represents two sciences in one: a biogeography absorbed into a therapeutics” (55).
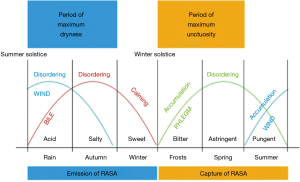
Time, which is unambiguously defined by two sets of three seasons (ṛtu)10 starting respectively with the summer and the winter solstice, is of the utmost importance in predicting the behavior of the three doṣas and therefore developing an efficacious therapeutic plan11. This explains the importance of living a balanced life in harmony with nature as well as one’s own social space. The figure below, derived from Vāgbhaṭa’s maxim: “Accumulation, disordering and calming take up three seasons, for wind those which begin with the summer, for bile those which begin with the rains, for phlegm those which begin with the frosts” (AHS i.12.24-25), summarizes at best this relation (55) (Figure 1):
As for land (deśa), this is uniquely defined by three kind of soils which in turn permit to classify food, to identify the most suitable physical activity and, more importantly, to prepare drugs. Though Caraka too addressed this issue (CaS i.27.332-333), it is Suśruta who first detailed it with greater articulation:
“The place is ānūpa, jāṅgala, or sādhāraṇa.
Ānūpa: the place characterized by an abundance of waters, the uneven terrain, rivers, rains and forests the softness and freshness of the winds, the abundance and height of the mountains and trees; the bodies of its men are soft, delicate and fat, disorders of phlegm and wind predominate.
Jāṅgala: the free, flat place characterized by sparsely scattered or rare thorny shrubs, a scarcity of water, rains, running water and wells, the heat and harshness of the winds, the sparsely scattered or rare rocks; the bodies of its men are tough and dry, disorders of wind and bile predominate.
Sādhāraṇa, the place which presents characteristics of both the others at once. Because, in a sādhāraṇa place, the cold, the rain, the heat and the wind are equal and the people enjoy an equality of humors, for that reason it is conceived as sādhāraṇa. The humors are no longer so strong, originating in the water and transplanted into a dry terrain, or else the converse, for they accumulate in their own place but fail to gain in intensity in another. Whoever behaves in a suitable fashion has nothing to fear from the place, his ways of feeding, sleeping and moving his body, etc., have all the qualities of that place.” (SuS i.35.42-47, translation by F. Zimmerman).
Beside its structural subdivision, place (deśa) is more generally considered of two kinds: the land (bhūmi) and the body (deha) (AHS i.1.23ab). It so appears that the vaidya should “create a doubly appropriate relationship: to render the environment appropriate to the needs of the patient and, conversely, to render the regimen of the patient appropriate to the ecological conditions.” (55). In doing so he interprets diseases as a series of factors which may weaken, aggravate or disrupt the balance of humors and tissues and, as a consequence, the relation between self (ātman), space (deśa) and time (kāla).
After advice on daily and seasonal regimen, medical compendia insist on the benefit of adequate physical exercise (śarīraceṣṭā), defined as “intentional movement of the body undertaken to gain firmness and an increase in strength” (CaS i.7.30). This is further corroborated by such hygienic norms as bathing, massaging, appropriate choice of clothes (which must be always clean) and diet (āhāra).
Whether we talk of cuisine or pharmacology, two sciences that often overlap (CaS i.26.12), Āyurvedic treatises carefully evaluate the proprieties of plants, herbs, animal products, metals and minerals as well as the way in which they are combined (saṃyoga). To such end, nighaṇṭus, glossaries of materia medica, were redacted from the 10th century12. Since drugs and foodstuff compensate for what the patient lacks (CaS i.1.62), the physician should be familiar with the constitution (prakṛti or svabhāva) and the requirements of his patient (upayoktṛ, lit. “one who enjoys [food]”) but also with the nature of foodstuff, the ways in which ingredients should be prepared (karaṇa), the place (deśa) where they are sourced and their seasonality (kāla). Next, he should consider the principles of pharmacology, namely the theory of savors (rasa). According to such scheme, each and every ingredient has the potential to be beneficial, toxic or capable to maintain the correct equilibrium. This depends on the ways in which substances react based on their qualities (guṇa)13 and savors (rasa)14 (58,59). However, as outlined in an important article by Dominik Wujastyk, the world (jagat) can be seen as an ecosystem revolving around basic opposites, namely agni and soma (60), fire and water, hot and cold, red and white, parched and nourished. Āyurveda too, with its strong emphasis on the relations between the environment and the various classes of beings inhabiting it, reflects this view. It is thus not unlikely that Indian medical authorities developed pharmacological principles as well as ideas on body, health and diseases moving from the concept that wellbeing derives from the exchanges between basic watery and fiery categories.
This brief survey, far from being exhaustive, demonstrates how Āyurveda has always privileged a holistic approach in which (I) anatomy and physiology, (II) pathology, diagnostics and prognostics and (III) therapeutics require a high degree of flexibility to develop unique strategies to the unique nature and (personal, social and cultural) circumstances of patients vis-à-vis the ever changing features of the environment in which they live. Yet eventually, as Agniveśa first cautioned us, any human being is ultimately responsible for their own pleasure (sukha) and pain (duḥkha) (CaS ii.7.22).
Bichat’s and Wirchow’s models: the dawn of “modern medicine”
The (Italian) National Bioethics Committee in 2001 defined medicine as “the art and science of diagnosis, treatment of disease, as well as maintenance of health” (61). In this brief definition different conceptual directions are condensed. These conceptual directions have been intertwined in the history of medicine in perennial opposition We refer to the “rationalist-mechanistic-reductionist-technical-fundamentalist/dogmatic” line of thought, which developed in the West World after Virchow and the “vitalist-empirical-systemic” (62)—typical line of traditional medicines but also the thought of Bichat.
The traditional Morgagni-Bichat-Virchow “genealogy” is presented in all the Manuals of History of Medicine (63) as a key center allowing medical knowledge to acquire “certain”/“scientific” bases about the organization of the human organism and about the passage from a state of health to one of disease (pathophysiology). This interpretation does not express the profound epistemological differences between the three great authors of biomedical thought at the turn of 1600–1800 BC and offers a distorted view of biomedical science as linear knowledge solidly founded on descent into the ever smaller. It means filtering history already starting with a mechanistic/reductionist lens. Presenting the transition from the organ (Morgagni) to the tissue (Bichat) and the cell (Virchow) as fundamental to proceed from a supposed “generic” and “pre-scientific” vision to a “precise” and “scientific” supposed one is anachronistic and misleading. In truth, as Bottaccioli (64) describes, Bichat does not study the tissue as a smaller and therefore “more detailed” and “more precise” level of the organ. The problem between Morgagni and Bichat does not concern the dimensions (macro/micro) nor the location of the pathology (organ/tissue). Bichat wanted to change “the way of considering pathological anatomy” (65), against Morgagni’s “topographical logic”, proposing to analyze the affections common to each system to then see the specificity of the organ. He proposed to contextualize the disease of an organ focusing on the systematic intertwining of the different tissues composing it.
Bichat did not want to found a “mechanistic” histology but, on the contrary, his scientific program envisaged the construction of a medicine that contemplates the localization of the disease in a systemic physiological framework. Here the difference towards Morgagni and Virchow is clear. The German pathologist considered the organism as a “federation of cells” where the cell itself, like a monad, determines the whole balance between health and disease (64). From this point of view, there is no linearity between Bichat and Virchow, but a profound diversity of scientific, systemic-French- and reductionist-German- model. Two models that are still contending the guidance of science and medical practice.
Einstein said: “It is the Theory that allows you to observe Reality.” There are no facts without their interpretation. And from a certain way of observing reality derives a certain way of interacting with it.
Thus it has been speculated that doctors/researchers from Virchow onwards, who believe in the “rationalist-mechanistic-reductionist-technical-fundamentalist” model may be seen as focused mostly in mechanistic aspects, may consider science in its exclusive technical sense. According to this rather dogmatic view, human beings can be “technicalized” and calculated and a pathological process represents a deviation from statistical “normality” or a “defect” which, in the history of medicine, was first located in organs, then in cells or in one or more molecules and currently in DNA. The human being is a linear sum of parts. There are single necessary and sufficient causes of disease, which are defined as a “pathological state” that must be quantified. If a part does not work, it needs to be repaired or replaced. It may not be very useful to invest in prevention, because in any case a machine will sooner or later break because of wear. If men are machines composed of similar parts, then “logical” and “possible” are considered only standardized treatments using similar dosages of drugs against personalized treatments. Following this thinking, the need for super-specialization of knowledge and for “treatment protocols” derives. Case of non-compliance with protocols may have legal consequences and generate the so called defensive medicine.
The Bichat-type physician/researcher, with an empiricist-systemic orientation, instead, is mostly a reader, an artist (66), considers science as a process of knowledge in progress in its theoretical as well as technical form. He is a prudent scientific being, aware of the problematic nature of the concept of “cause”. He is aware of its only probable knowledge and therefore constantly tries to “investigate” the single human being in front of him and the processes that involve him before using pre-defined “labels” (67). The interaction between multiple elements reveals properties that cannot be explained by the individual elements of the system. As Aristotle already said: “the human being is more than the sum of its parts”. The human being is a chaotic and complex network of dynamic processes. Crucial for disease development are alterations of the relationship between the individual with himself and his environment, the lifestyle, the psychological dynamics. Disease development is a progressive process with a network of contributing causes that may be necessary but not sufficient alone to determine the final phenomenon. As in the ancient medicines, space is given to the quantitative but also qualitative study of natural phenomena. A sick person needs to be brought back into balance. In fact, a “sick car” can have all the parts in order but a bad driver who is responsible for the “dysfunction”. Prevention and rehabilitation is the foundation of this type of vision of man and life (68,69). Individuals are different and specific and the therapy must be individualized (70). The specialization of knowledge and the observations obtained from the study of a population must be relativized in front of the single case that the doctor has in front of him and which may not fall within “rigid statistical parameters” (71,72).
Psycho-neuroendocrine-immunology, epigenetics and Biophysics as a possible integration model
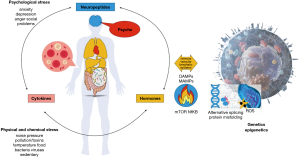
If we consider Hans Selye’s studies on stress (73), the discovery of the multi-organ crosstalk between the nervous, endocrine and immune systems via neurotransmitters, cytokines and hormones (74,75) but also the notion that biological phenotypes are influenced by stable, reversible and heritable epigenetic modulation of DNA (76), then biological reductionism may appear an obsolete epistemological and therapeutic paradigm (77). The “normal” thresholds may be questioned (71,72) as health or illness of a human being actually represent the result of the relationship with himself and with the environment (78,79).. Alongside the advent of Psycho-neuroendocrine-immunology and Epigenetics (Figure 2), new evidence in the biophysical field is further shifting the scientific center of gravity from the “chemistry point of view” to the “physical point of view” of the human being. Many biological processes are too rapid (90,91) to be explained by chemical diffusion mechanisms based on stochastic variations of solute concentrations or ligand-receptor dynamics. Ondulatory oscillating processes, long-range molecular interactions involving water (92,93), interactions of weak electromagnetic fields (94), cellular behavior regulation thanks to acoustic waves (95) represent the new frontier of biomedical research. And, probably, they will allow a greater understanding of those ancient knowledge, very refined, but expressed in a language classified as “symbolic” by a “modern man”.
The complexity of nature and of physiological and pathological phenomena is evident, but medicine still needs to draw further adequate methodological consequences from it. In clinical medical practice a reductionist, hyper-specialist and technological, “drug-centric” way is seen. Guidelines and protocols, which are merely focused on (96) statistics erroneously understood as an instrument of “truth” (97,98) can clash with multiform reality (89,96-103). The “etiological therapy” postulates the existence of a single cause deemed necessary and sufficient to explain a pathological process. This is a pre-requisite for “gene therapy” or “antiviral therapy”. This may certainly a useful approach in many cases, however not always. Studies of twins very often show different phenotypic results with the same genome (103) or asymptomatic/not infected subjects are present when exposed to a common infectious agent. There is the symptomatic “suppressive therapy”, typical of pharmacological mechanisms and the “replacement therapy”, “amputative” or “reparative” therapies as in the case of surgery. Some researches described that 30–36% of patients are suffering from iatrogenic diseases (104,105) and from “consolidated therapy” (106-109).
There is one last form of therapy, typical of ancient medicine and modern clinical practice, albeit still a minority: the “regulatory” therapy of the single patient. In Integrative Medicine (110,111) the patient is placed at the center of an intervention program. The aims are to re-balance and regulate a series of neuro-endocrine-immune and biophysical networks under tension, proceeding with food changes, physical (physical exercise, massage, acupuncture), climatic-environmental, psychological (mind-body techniques) stimulations along with evidence-based phytotherapy (112-114). It is curious to note that according to the perspective of ancient medicine those symptoms commonly recognized as “mild” or “initial” from “modern doctors” are instead considered by the “preventive view” of ayurvedic physicians the last stages leading to a disease manifestation (114).
A successful combination between traditional and modern medicine: the example of plants use
The fundamental difference between traditional and contemporary medicine lies in the subjective approach to the reality of the former in comparison to the more objective approach of the latter. These two modes are not incompatible as shown for instance in the use of an herb as seen by the modern and traditional medicine/pharmacology.
As described by Schrott and Ammon (115), Althaea officinalis Linn—marsh-mallow—it’s a common Malvaceae plant in Europe and Asia. Roots and flowers are used for medical applications. It is sweet, oily, slimy, heavy, cold and it is used mostly as a nourishing pulmonary tonic. It is expectorant, diuretic, laxant and an emollient remedy for stomach and intestine (for its mucilagues). It is used in inflammatory diseases of the lungs and intestine and in dyspepsia, vaginal inflammations, dysuria and urinary infections, mastitis, skin ulcers, rheumatic problems and in states of emaciation (112). Interestingly, in Ayurveda the same use is described (115).
How is that possible? Ancient doctors used to classify the substances based on their qualities: sweet, salty, bitter, astringent, pungent, sour. Modern scientists look rather at the chemical composition of substances by identifying proteins, carbohydrates, etc. in plants. It is interesting to note that mucopolysacarides, polysaccharides, diterpenes have a sweet taste; iridoides, cucrbitacines, quassinoides, saponines, alkaloids, some flavonoids, chinins or lignanes are bitter; tannins are astringent, piperin, capsaicin or gingerol are pungent and some acids or essential oils are sour (115). Moreover, saponines (mainly bitter taste) have an anti-inflammatory, antiviral, antimicrobial, antipyretic, diuretic and hepatoprotective, hypoglycemic and hypolipidemic, anti-tumoral action (112,115).
For thousands of years ancient doctors used subjective perception about the qualities of the constitutive elements to deduce the therapeutic effect of the substances with great precision. Proceeding with perceptions, observations, trials and errors they selected the most effective remedies for their contemporary human beings. Modern technical experimentation has a very young history but may reach [attention to the epistemological limits of technical-scientific research (116)] often similar conclusions as the men who preceded us (115).
A dialogue with traditional medicine is possible in different medical fields
As discussed earlier, the specialization of knowledge is undoubtedly a wealth, but ideally this should be integrated with a systematic overview. In this regard, it may be certainly advantageous to observe “the patient through the heart”, but it would be a conceptual and clinical error to look at the heart, without considering the patient as a whole.
Increasing evidence favor an integrated treatment of various pathological conditions, able to alleviate suffering of people and to reduce healthcare costs (110,117). In addition to the well-known positive effects of healthy eating (118), exercise and smoking cessation (110), the use of herbal medicine (112) and mind-body disciplines seem to be particularly important. For instance, stress as contributor of different pathological states can be ameliorated through different nutritional and phyto-therapeutic, physical or psychological stimulations (119).
Below some interesting examples of cooperation between traditional and modern medicine.
Heart diseases
Often depression and dyslipidemias are present together. From a reductionist’s point of view this co-existence may be seen as coincidental and will be treated with a lipid-lowering drug combined with an anti-depressive pill. From a different perspective, depression and dyslipidemias may result from a psychological imbalance with (chronic) inflammation leading to dyslipidemia and depression. In fact, high anxiety and stress levels may lead to higher LDL cholesterol levels. Effort, over-commitment, low reward and effort-reward imbalance are significantly associated with increasing blood lipids and are suggested as a possible link between job stress and coronary heart disease (120).
Furthermore, chronic stress may impair vascular function (121). We have seen that depression (and dyslipidemia) are linked to a pro-inflammatory regulation of the immune system (122,123). Hence, psychosocial factors may act as cardiovascular risk factors along with the well-established ones (i.e., smoke, dyslipidemia, hypertension and obesity) (124). Thus psychosocial factors should be taken into account for the prevention of heart disease (125,126). As confirmed by evidence linking depression in absence of additional risk factors to coronary artery calcification (127).
Starting from these backgrounds, we studied the impact of stress on cardiovascular diseases (76,86,128-135) and we applied some “traditional” knowledge to treat patients after myocardial infarction. Thanks to proper nutrition (Mediterranean diet) and food supplementation (131), to mild-moderate aerobic exercise (131) and stress management (through the use of mind-body disciplines as listening of music or meditation) we observed an initial regression of carotid atherosclerosis and improvement in coronary flow (136),as suggested also by others (137-143). We documented also significant variations of stress hormones, inflammatory (136), and epigenetic markers (144) with simple biophysical and biochemical explanations (95,145).
Infective diseases
Chronic psychosocial stressors are related to alterations in inflammatory activity. Job stress, low socioeconomic status, childhood adversities as well as life events, caregiver stress, and loneliness were shown to augment Th2 response while decreasing Th1 thus influencing the immune response. An interesting study by Rosenkranz et al. reports relations among physiological measures of affective style, psychological well being, and immune function. Negative and positive feelings were elicited by using an autobiographical writing task. Individuals characterized by a more negative affective style mounted a weaker immune response which may relate to higher susceptibility for illness as compared to those with a more positive affective style (146). Furthermore, stress reduction behavioral interventions, such as Tai Chi, enhances vaccine-stimulated levels of cell-mediated immunity to varicella zoster virus (147). Stress increases HIV disease progression (148).
A proper nutrition also supports the immune system (110,117) as well as mild to moderate physical activity (149,150). Several plants exert antiviral, antibacterial and antiparasitic properties (such as Astragalus Membranaceus, a plant used in Chinese medicine), Whitamnia Somnifera (used in ayurvedic medicine), Liquorice (used in Mediterranean medicine), Allium sativum, Zingiber officinalis etc.) (112).
Probably, considering these factors may help to decrease susceptibility to certain infections keeping a healthy immune system. This could be an important consideration in drawing realistic epidemiological mathematical models and for the prevention of infections in the population [a current world-wide issue where the integration of phytotherapy and nutritional supplements seem to be a valid tool to be further investigated (151-157)].
Cancer
Chronic behavioral stress results in higher levels of tissue catecholamine, greater tumor burden and more invasive growth of carcinoma cells in animal models (158) and in humans (159). Behavioral factors contribute to the crosstalk between tumor and host cells in the tumor microenvironment, and stress effects on host cells such as macrophages seem to be critical for many pathways involved in tumor progression. Some effects are bidirectional in that tumor-derived inflammation seems to effect central nervous system processes, triggering vegetative symptoms and contributing to deregulation of the hypothalamic-pituitary-adrenal axis with downstream effects on inflammatory control (160).
Depression and social isolation seems to play an important role in cancer spreading (161,162). treating depression can prolongs life in cancer patients (160). A randomized clinical trial tested the hypothesis that cancer patients coping with their recent diagnosis and receiving psychological help improved survival time compared with patients, who only received the diagnosis (163). Additionally, mindfulness based stress reduction for women recently diagnosed with early stage breast cancer showed beneficial effects on immune function with an increase in Th1 INFγ levels, enhanced quality of life, and coping with the disease (164). Also in cancer patients the immune system may be strengthened through an adequate nutritional regimen (117), physical activity (117) and the use of natural immuno-stimulants with possible anti-tumor action (i.e., Artemisia annua) (112,117).
Skin diseases
It is well known that skin cells produce stress hormones (165) and a “brain-skin connection” underlying inflammatory skin diseases may be triggered or aggravated by stress (166). Psoriasis lesions disappear when CRH and nervous growth factor (NGF) levels from nervous skin terminals decrease turning off mast-cells activity (167). As recognized by ancient medicine (29,38), many dermatological problems are affected by intestinal problems or food allergies (110,117). A proper nutrition may alleviate skin problems.
Multiple sclerosis
A relationship in the distribution of multiple sclerosis with latitude and solar radiation was described (168), with higher incidence of the disease in northern countries (169). It is interesting to notice that migrating to areas with higher sun exposition decreases the incidence of the disease (170). Probably these findings are related to the Vitamin D stimulating action on the Th2 immune circuits, decreasing the production of Th1-related cytokines (i.e., TNFα and INFγ) (75). Furthermore Buljevac et al. demonstrated that stressful events are associated with increased exacerbations in relapsing-remitting multiple sclerosis and this association was independent of the triggering effect played by of infections (171) but rather be related to the noradrenaline-dependent adrenergic stimulation activation of the pro-inflammatory gene NF-kappa B in monocytes elicited by stress (172). Again the immuno-modulatory action of some foods, phyto-therapy, physical activity and mind-body techniques can be exploited this disease (75,173).
Rheumatic diseases
Psychological stress acting via hormonal and neuronal stimuli may exacerbate rheumatoid arthritis (174). Cognitive behavioural interventions, offered as an adjunct to standard clinical management early in the course of rheumatoid arthritis, is efficacious in improving psychological and physical disease aspects (175). Association of fasting and vegetarian diet is an effective integrative treatment for rheumatoid arthritis (176). Similar findings are reported for lupus erythematosus too (177,178) and behavioral interventions designed to reduce emotional reactivity may be of therapeutic benefit in chronic inflammatory conditions in general, such as neurogenic inflammation (179).
Conclusions
Integrative medicine bringing together a healing-oriented and patient-centered sensibility with therapeutic approaches originating from “alternative” and “traditional” medicine may help improving contemporary medicine. Integrative medicine is increasingly recognized as strategic against the epidemic of chronic diseases, which pose a serious concern on health care systems. Further research in this field is needed to further enable contemporary medicine to adopt a systemic perspective based on psycho-neuro-endocrine-immunology connections and epigenetics.
Acknowledgments
Funding: EO is supported by the Swiss National Science Foundation (PRIMA: PR00P3_179861/1), the Swiss Life Foundation, the Heubergstiftung and the Swiss Heart Foundation, Switzerland.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/lcm-20-27
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/lcm-20-27). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
1Although there is abundant evidence of a healing culture in earlier Vedic civilization, texts like Ṛgveda, Atharvaveda and the later Kauśikasutra bear witness to a form of medicine which is primarily ritual.
2The core sections of the Carakasaṃhitā and the Suśrutasaṃhitā should be dated back respectively to 500 BCE and before 250 BCE.
3To Vāgbhaṭa is also attributed the Aṣṭāṅgasaṃgraha and, among the others, the iatro-chemical treatise known as Rasaratnasamuccaya.
4There exist other texts whose original sections might be as early as Carakasaṃhitā (on internal medicine) and Suśrutasaṃhitā (on surgery). Amongst these, the Bhelasaṃhitā (45) and the Kāśyapasaṃhitā (46) (on obstetrics, gynecology, and pediatrics), both fixated in their actual form between the 4th and the 7th centuries CE. For an exhaustive census and analysis of āyurvedic works, see Meulenbeld’s encyclopedic A history of Indian medical literature (47).
5CAS I.8.15-16.
6CAS I.11.37, ASAṂ I.22.7.
7In SUS III.5.3, Suśruta considers the formation of the embryo as resulting from semen (śukra), blood (śoṇita), the self (ātman), nature (prakṛti) and consciousness (cetanā).
8The pañcamahābhāta, i.e. air (ākāśa), wind (vayu), fire (agni), water (āpaḥ) and earth (pṛthivī),
9The wind is primarily located in the intestine, the bile/choler in the navel, and the phlegm in the chest.
10Vasanta (Spring), Grīṣma (hot season), Varṣā (rainy season), Śarad (Autumn), Hemanta (Cool season) and Śiśira (Winter).
11See Cakrapāṇidatta’s Āyurvedadīpikā ad CAS I.1.54.
12The most important glossaries of materia medica are the Dhanvantarīyanighaṇṭu, the Rājanighaṇṭu, the Madanapālanighaṇṭu and the Bhāvaprakāśanighaṇṭu (56,57).
13Qualities are listed as ten opposites, namely heavy (guru) and light (laghu), slow (manda) and fast (tīkṣṇa), cold (hima) and hot (uṣṇa), unctuous (snigdha) and dry (rūkṣa), smooth (ślakṣṇa) and rough (khara), solid (sāndra) and liquid (drava), soft (mṛdu) and hard (kaṭhina), stable (sthira) and mobile (cala), subtle (sūkṣma) and gross (sthūla), non-slimy (viśada) and slimy (picchila) (CAS III.6.10; SUS I.40.10-12; AHS I.9).
14Āyurvedic pharmacology is built on four concepts: (I) six basic savors: sweet (madhura), sour (amla), salt (lavaṇa), bitter (tikta), pungent (kaṭu) and astringent (kaṣāya); (II) modified post-digestive (vipāka) savors; (III) potency (vīrya), i.e. the ability to resist to digestive fire; and (IV) special potency (prabhāva), which serves to justify exceptions (AHS I.1.14-18).
References
- Jouanna J. Hippocrate. Paris: Librarie Arthème Fayard, 1992.
- Nutton V. Ancient Medicine 2nd ed. London - New York: Routledge, 2013.
- Craik EM. The ‘Hippocratic Question’ and the Nature of the Hippocratic Corpus. In: Pormann PE. The Cambridge Companion to Hippocrates Cambridge: Cambridge University Press, 2018:25-37.
- Pormann PE. The Cambridge Companion to Hippocrates. Cambridge: Cambridge University Press, 2018.
- Hanson AE. Hippocrates: Diseases of Women I. Signs (Chic) 1975;1:567-84. [Crossref] [PubMed]
- Grmek MD. Les maladies à l’aube de la civilisation occidentale. Paris: Payot, 1983.
- Kingsley P. Ancient Philosophy, Mystery, and Magic: Empedocles and Pythagorean Tradition. Oxford: Oxford University Press, 1995.
- Dobson JF. Herophilus of Alexandria. Proc R Soc Med 1925;18:19-32. [Crossref] [PubMed]
- Garofalo I. Erasistrati fragmenta. Pisa: Giardini, 1988.
- Von Staden H. Herophilus. The Art of Medicine in Early Alexandria. Cambridge - New York: Cambridge University Press, 1989.
- Vegetti M. Tra il sapere e la pratica: la medicina ellenistica. In: Grmek MD. ed Storia del pensiero medico occidentale. 3 vols. Bari: Laterza 1993:73-120.
- Longrigg J. Anatomy in Alexandria in the Third Century B.C. Br J Hist Sci 1988;21:455-88. [Crossref] [PubMed]
- Jones WHS. The Medical Writings of the Anonymous Londinensis. Cambridge: Cambridge University Press, 1947.
- Leith D. Erasistratus’ triplokia of arteries, veins and nerves. Apeiron 2015;48:251-62. [Crossref]
- Hankinson RJ. editor. The Cambridge Companion to Galen. Cambridge: Cambridge University Press, 2008.
- Galenism TO. Rise and Decline of a Medical Philosophy. Ithaca: Cornell University Press, 1973.
- Singer PN. Galen: Selected Works: Translated with an Introduction and Notes. Oxford - New York: Oxford University Press, 1997.
- Garofalo I, Vegetti M. Opere scelte di Claudio Galeno. Torino: UTET, 1978.
- Vegetti M. Galeno e la rifondazione della medicina. Dynamis Acta Hisp ad Med Sci Hist Illus 1995;15:67-101.
- Van der Eijk P. Therapeutics. In: Hankinson RJ. Editor. The Cambridge Companion to Galen Cambridge: Cambridge University Press, 2008:283-303.
- Unschuld PU. Introductory Readings in Classical Chinese Medicine. Sixty Texts with Vocabulary and Translations, a Guide to Research Aids and a General Glossary. Dordrecht - Boston - London: Kluwer Academic Publisher, 1998.
- Xiu HZ. The materialistic theory of Yuan Qi - One of the brilliant philosophical ideas of the legal school. Sci Sin 1968;18:697-704.
- Needham J. Science and Civilization in China. Cambridge: Cambridge University Press, 1956.
- Granet M. La Pensée chinoise. La Reinassance du Livre: Paris, 1934.
- Lozano F. Basic theories of Traditional Chinese Medicine. In: Yuan-Chi L, Shen-Zen Hsu E. editors. Acupuncture for Pain Management Heidelberg - Dordrecht - London - New York: Springer, 2013:13-43.
- Wuxing HJ. Five Phases. In: Cua AS. editor. Encyclopedia of Chinese Philosophy New York: Routledge, 2003:786-8.
- Rochat de la Vallee E. Wuxing: The Five Elements in Classical Chinese Texts. London: Monkey Press, 2009.
- Zhang H, Sun Y, Gao Z, et al. A disturbance rejection framework for the study of Traditional Chinese Medicine. Evid Based Complement Alternat Med 2014;2014:787529 [Crossref] [PubMed]
- Maciocia G. The Foundation of Chinese Medicine. 3rd ed. New York: Elsevier, 2015.
- Loukas M, Ferrauiola J, Shoja M, et al. Anatomy in Ancient China: The Yellow Emperor’s Inner Canon of Medicine and Wang Qingren’s Correcting the Errors in the Forest of Medicine. Clin Anat 2010;23:364-9. [Crossref]
- Veith L. Huang Ti Nei Ching Su Wên. Berkeley: University of California Press, 1976.
- Barnes LA, Hinrichs TJ. Introduction. In: Hinrichs TJ, Barnes L. editors. Chinese Medicine and Healing Cambridge MA. London: The Belknap Press of the Harvard University Press, 2013:1-4.
- de Lima Pimentel R, Duque AP, Moreira BR, et al. Acupuncture for the treatment of cardiovascular disease: a systematic review. J Acupunct Meridian Stud 2019;12:43-51. [Crossref] [PubMed]
- Lupi G, Cormio M. Acupuncture in Cardiovascular Diseases. In: Fioranelli M. editor. Integrative Cardiology A New Therapeutic Vision. New York: Springer, 2017:39-52.
- Lo V. The Han Period. In: Hinrichs TJ, Barnes L. editors. Chinese Medicine and Healing Cambridge MA. London: The Belknap Press of the Harvard University Press, 2013:31-64.
- Tseng Y, Chao C, Hung Y, et al. Efficacy of Stimulation at the Jing-Well Points of Meridians. Int J Nurs Clin Pract 2015;2:121. [Crossref]
- Cook CA. The Pre-Han Period. In: Hinrichs TJ, Barnes L. editors. Chinese Medicine and Healing Cambridge MA. London: The Belknap Press of the Harvard University Press, 2013:5-29.
- Agniveśa’s Caraka Saṃhitā. Text with English Translation & Critical Exposition Based on Cakrapāṇi Datta’s Āyurveda Dīpikā by R.K. Sharma and B. Dash. 7 vols. Varanasi: Chowkhamba Sanskrit Series Office; 1976. (Chowkhamba Sanskrit Studies, no. XCIV).
- Suśruta-saṃhitā with English Translation of Text and Ḍalhaṇa’s Commentary along with Critical Notes by P.K. Sharma. 3 vol. Varanasi: Chaukhambha Visvabharati; 1999. (Haridas Ayurveda Series, no. 9).
- Vāgbhaṭa’s Aṣṭāñga [sic] Hr̥daya. Text, English Translation, Notes, Appendix and Indices by R.K. Srikantha Murthy. 3 vols. Varanasi: Krishnadas Academy; 1991. (Krishnadas Ayurveda Series, no 27).
- Vāgbhaṭa’s Aṣṭāṅgahṛdayasaṃhitā. The first five chapters of its Tibetan version. Edited and rendered into English along with the original Sanskrit by Claus Vogel. Accompanied by a literary introduction and a running commentary on the Tibetan translating-t.
- The Mādhavanidāna: with ‘Madhukośa’, the commentary by Vijayarakṣita and Śrīkaṇṭhadatta (ch 1-10). Introduction, Translation and Notes by GJ. Meulenbeld 1st Ind. ed. Delhi: Motilal Banarsidass Publishers; 2008. 709 p. (Indian medical tradition, no. I.
- Sārṅgadhara [sic]-Saṃhitā. A treatise on Āyurveda. Translated in English KR. Srikantha Murthy. Reprint. Varanasi: Chaukhambha Orientalia; 2001. (Jaikrishnadas Ayurveda Series, no. 58).
- Bhāvaprakāśa of Bhāvamiśra: text, English translation, notes, appendences [sic] and index by KR Srikantha Murthy 2 vols. Varanasi: Chowkhamba Krishnadas Academy; 2001. (Krishnadas Ayurveda Series 45).
- Bhela-Saṃhitā. Text with English Translation, Commentary and Critical Notes by KH. Krishnamurthy and edited by PV. Sharma. Varanasi: Chaukhambha Visvabharati; 2000. (Haridas Ayurveda Series, no. 8).
- Kāśyapa-saṃhitā or Vr̥ddhajīvakīya Tantra. Preached by Maharṣi Mārica Kaśyapa; summarized then written by his disciple Ācārya Vr̥ddhaJīvaka; redacted by latter’s descendant Vātsya. Text with English Translation and Commentary by PV. Tewari. Reprint. Varan.
- Meulenbeld G. A History of Indian Medical Literature. 5 vols. Groningen: Forsten, Egbert, 1999.
- Jolly J. Medicin. Strassburg: Trübner; 1901. (Grundriss der indo-arischen Philologie und Altertumskunde, Bd. 3, Heft 10).
- Müller R. Über die Tridoṣa-Lehre in der altindischen Medizin. Sudhoffs Arch für Geschichte der Medizin und der Naturwissenschaften 1939;32:290-314.
- Scharfe H. The Doctrine of the Three Humors in Traditional Indian Medicine and the Alleged Antiquity of Tamil Siddha Medicine. J Am Orient Soc 1999;119:609-29. [Crossref]
- Moriguchi M. The concept of diseases and the tri-doṣa theory in the Suśrutasaṃhitā. J Indian Buddh Stud 2015;63:1183-90. (Indogaku Bukkyogaku Kenkyu).
- Hilgenberg L, Kirfel W. Vāgbhaṭa’s Aṣṭāṅgahṛdayasaṃhitā, ein altindisches Lehrbuch der Heilkunde, aus dem Sanskrit ins Deutsche übertragen mit Einleitung, Anmerkungen und Indices. Leiden: E.J. Brill, 1941.
- Maas P. Indian Medicine and Ayurveda. In: Jones A, Taub L. editors. The Cambridge History of Science Volume 1: Ancient Science Cambridge: Cambridge University Press, 2018:532-49.
- Wujastyk D. editor. The Roots of Ayurveda: selections from Sanskrit medical writings. Rev. ed. London; New York: Penguin Books (Penguin classics), 2003.
- Zimmermann F. The Jungle and the Aroma of Meats. An Ecological Theme in Hindu Medicine. Delhi: Motilal Banarsidass, 1999.
- Nārāyaṇaśarma VeŚāRāRā ‘Puraṃdare’. editor. Rājanighaṇṭusahito Dhanvantarīyanighaṇṭuḥ. Puṇyākhyapattana: Ānandāśramamudraṇālaya; 1986. (Ānandāśramasaṃskr̥tagranthāvali, no. 33).
- Madanapāla. Materia Medica of Ayurveda Based on Madanapāla’s Nighaṇṭu. Dash B, Gupta K, editors. New Delhi: Jain Publishers 2001.
- Wujastyk D. The combinatorics of tastes and humours in classical Indian medicine and mathematics. J Indian Philos 2000;28:479-95. [Crossref]
- Meulenbeld G. Reflections on the basic concepts of Indian pharmacology. In: Meulenbeld GJ, Wujastyk D. editors. Studies in Indian Medical History Delhi: Motilal Banarsidass, 2001:1-16.
- Wujastyk D. Agni and Soma: a universal classification. In: Ciurtin E, editor Du corps humain, au carrefour de plusieurs savoirs en Inde: mélanges offerts à Arion Rosu par ses collègues et ses amis à l’occasion de son 80° anniversaire = The human body, at the crossroads of multiple Indian ways of knowing: papers 2003. p. (Stvdia Asiatica, IV-V) 347-69.
- Bellavite P. Medicine: therapeutic art and experimental science. J Med Person 2006;4:157-62.
- Israel G, Roma D, Sapienza L. Medicine between humanism and mechanism. La medicina tra umanesimo e meccanicismo. J Med Pers 2008;6:5-13.
- Angeletti LR, Gazzaniga V. Storia, filosofia ed etica generale della medicina. II. Masson, editor. Milano; 2004.
- Bottaccioli F. Due vie per la medicina scientifica al suo sorgere. I. Aracne, editor. Roma; 2013.
- Bichat FX. Anatomie générale appliquée a la physiologie et a la médicine. Broson, editor. Paris; 1801.
- Wulff HR, Pedersen SA, Rosemberg R. Philosophy of Medicine. Blackwell Scientific Pubblications; 1986.
- Crick F. Central dogma of molecular biology. Nature 1970;227:561-3. [Crossref] [PubMed]
- Bobbio M, Abrignani MG, Caldarola P, et al. “Fare di più non significa fare meglio”. Le proposte dell’ ANMCO. G Ital Cardiol 2014;15:244-52.
- Bobbio M, Galvagno G. Nuove diagnosi senza nuovi trattamenti. G Ital Cardiol 2014;15:289-92.
- Schork NJ. Personalized medicine: Time for one-person trials. Nature 2015;520:609-11. [Crossref] [PubMed]
- Giannoni A, Baruah R, Leong T, et al. Do optimal prognostic thresholds in continuous physiological variables really exist? Analysis of origin of apparent thresholds, with systematic review for peak oxygen consumption, ejection fraction and BNP. PLoS One 2014;9: [Crossref] [PubMed]
- McCormack J, Vandermeer B, Allan GM. How confidence intervals become confusion intervals. BMC Med Res Methodol 2013;13:134. [Crossref] [PubMed]
- McEwen BS. Protective and damaging effects of stress mediators: The good and bad sides of the response to stress. Metabolism: Clinical and Experimental 2002;51:2-4. [Crossref] [PubMed]
- Ader R. Psychoneuroimmunology, Two-Volume Set. Elsevier, 2011:1320 p.
- Bottaccioli F, Bottaccioli AG. Psiconeuroendocrinoimmunologia e scienza della cura integrata. Il manuale. Edra S.p.A; 2017. 720 p.
- Dal Lin C, Poretto A, Scodro M, et al. Coronary microvascular and endothelial function regulation: Crossroads of psychoneuroendocrine immunitary signals and quantum physics J Integr Cardiol 2015;1:132-209. [Part A-B and C].
- Strohman RC. The coming Kuhnian revolution in biology. Nat Biotechnol 1997;15:194-200. [Crossref] [PubMed]
- Yan Q. The role of psychoneuroimmunology in personalized and systems medicine. Methods Mol Biol 2012;934:3-19. [Crossref] [PubMed]
- Engel GL. The need for a new medical model: a challenge for biomedicine. Science 1977;196:129-36. [Crossref] [PubMed]
- Dal Lin C, Tona F, Osto E. The Heart as a Psychoneuroendocrine and Immunoregulatory Organ. In: Advances in experimental medicine and biology. 2018:225-39.
- Choudhuri S. From Waddington’s epigenetic landscape to small noncoding RNA: some important milestones in the history of epigenetics research. Toxicol Mech Methods 2011;21:252-74. [Crossref] [PubMed]
- Saxton RA, Sabatini DM. mTOR Signaling in Growth, Metabolism, and Disease. Cell 2017;168:960-76. [Crossref] [PubMed]
- Li X. NFκB-dependent signaling pathways. Exp Hematol 2002;30:285-96. [Crossref] [PubMed]
- Picard M, McEwen BS, Epel ES, et al. An energetic view of stress: Focus on mitochondria. Front Neuroendocrinol 2018;49:72-85. [Crossref] [PubMed]
- Macario AJL, Conway de Macario E. Stress and molecular chaperones in disease. Int J Clin Lab Res 2000;30:49-66. [Crossref] [PubMed]
- Pick M, Flores-Flores C, Soreq H. From Brain to Blood: Alternative Splicing Evidence for the Cholinergic Basis of Mammalian Stress Responses. Ann N Y Acad Sci 2004;1018:85-98. [Crossref] [PubMed]
- Matzinger P. An innate sense of danger. Semin Immunol 1998;10:399-415. [Crossref] [PubMed]
- Babenko O, Kovalchuk I, Metz GAS. Stress-induced perinatal and transgenerational epigenetic programming of brain development and mental health. Neurosci Biobehav Rev 2015;48:70-91. [Crossref] [PubMed]
- Guerrero-Bosagna C, Skinner MK. Environmentally induced epigenetic transgenerational inheritance of phenotype and disease. Mol Cell Endocrinol 2012;354:3-8. [Crossref] [PubMed]
- Wang N, Tytell JD, Ingber DE. Mechanotransduction at a distance: Mechanically coupling the extracellular matrix with the nucleus. Nat Rev Mol Cell Biol 2009;10:75-82. [Crossref] [PubMed]
- Muehsam D, Ventura C. Life rhythm as a symphony of oscillatory patterns: electromagnetic energy and sound vibration modulates gene expression for biological signaling and healing. Glob Adv Health Med 2014;3:40-55. [Crossref] [PubMed]
- Ball P. Water as an active constituent in cell biology. Chem Rev 2008;108:74-108. [Crossref] [PubMed]
- Del Giudice E, Voeikov V, Tedeschi A, et al. The origin and the special role of coherent water in living systems. In: Fels D, Cifra M, Scholkmann F. editors. Fields of the Cell 2015:95-111.
- Ventura C. Seeing Cell Biology with the Eyes of Physics. Nano World J 2017;3:S1-8. [Crossref]
- Dal Lin C, Radu C, Vitiello G, et al. In vitro effects on cellular shaping, contratility, cytoskeletal organization and mitochondrial activity in HL1 cells after different sounds stimulation. A qualitative pilot study and a theoretical physical model. bioRxiv 2020;2020.03.19.993618.
- Lepore J. It’s Spreading|The New Yorker. New Yorker, May 25 2009.
- Packer M. The Parable of Schrödinger’s Cat and the Illusion of Statistical Significance in Clinical Trials. Circulation 2019;140:799-800. [Crossref] [PubMed]
- Wasserstein RL, Lazar NA. The ASA’s Statement on p-Values: Context, Process, and Purpose. Am Stat 2016;70:129-33. [Crossref]
- Smith R. Peer review: A flawed process at the heart of science and journals. J R Soc Med 2006;99:178-82. [Crossref] [PubMed]
- Hausmann L, Schweitzer B, Middleton FA, et al. Reviewer selection biases editorial decisions on manuscripts. J Neurochem 2018;146:21-46. [Crossref] [PubMed]
- Fong EA, Wilhite AW. Authorship and citation manipulation in academic research. PLoS One 2017;12: [Crossref] [PubMed]
- Tancock C. When reviewing goes wrong: the ugly side of peer review [Internet]. Available online: https://www.elsevier.com/connect/editors-update/when-reviewing-goes-wrong-the-ugly-side-of-peer-review
- Gagel RF, McCutcheon IE. Pituitary Gigantism. N Engl J Med 1999;340:524. [Crossref] [PubMed]
- Steel K. Iatrogenic illness on a general medical service at a university hospital. Qual Saf Health Care 2004;13:76-80. [Crossref] [PubMed]
- Kramer MS, Hutchinson TA, Flegel KM, et al. Adverse drug reactions in general pediatric outpatients. J Pediatr 1985;106:305-10. [Crossref] [PubMed]
- . Need We Poison the Elderly So Often? Lancet 1988;2:20-2. [PubMed]
- Barie PS. Modern surgical antibiotic prophylaxis and therapy--less is more. Surg Infect (Larchmt) 2000;1:23-9. [Crossref] [PubMed]
- Bailar JC, Smith EM. Progress against Cancer? N Engl J Med 1986;314:1226-32. [Crossref] [PubMed]
- Winslow CM, Kosecoff JB, Chassin M, et al. The Appropriateness of Performing Coronary Artery Bypass Surgery. JAMA 1988;260:505-9. [Crossref] [PubMed]
- Rakel D. Integrative Medicine 3rd Edition. Elsevier, 2012.
- Maizes V, Schneider C, Bell I, et al. Integrative medical education: development and implementation of a comprehensive curriculum at the University of Arizona. Acad Med 2002;77:851-60. [Crossref] [PubMed]
- Fabio Firenzuoli. Fitoterapia. Guida all’uso clinico delle piante medicinali. Elsevier, 2009.
- Fioranelli M. Integrative Cardiology 1st ed. Fioranelli M, editor. Springer International Publishing. Cham: Springer International Publishing, 2017.
- Vaidya Dash B. Agniveśa’s Caraka Saṃhitā 7 Volumes set. Chowkhamba Sanskrit Series Office; 2009. 7 volumes set.
- Schrott E, Ammon HPT. Heilpflanzen der ayurvedischen und der westlichen Medizin: Eine Gegenüberstellung. Springer Berlin Heidelberg; 2012.
- Arló-Costa H, Hendricks VF, Johan van Benthem. Readings in Formal Epistemology. Springer graduate text in phylosophy. Cham: Springer International Publishing; 2016.
- Micozzi MaS. Complemenetary and alternative medicine. 5th ed. Elsevier; 2015.
- Dorigo A. Ciao, mangiamo insieme? L’alimentazione sana e di qualità per tutti. Ed. Mille, 2004.
- Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol 2009;5:374-81. [Crossref] [PubMed]
- Xu W, Hang J, Gao W, et al. Association between job stress and newly detected combined dyslipidemia among Chinese workers: findings from the SHISO study. J Occup Health 2011;53:334-42. [Crossref] [PubMed]
- Neves VJ, Moura MJCS, Almeida BS, et al. Chronic stress, but not hypercaloric diet, impairs vascular function in rats. Stress 2012;15:138-48. [Crossref] [PubMed]
- Dantzer R, O’Connor JC, Freund GG, et al. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci 2008;9:46-56. [Crossref] [PubMed]
- Dantzer R, Kelley KW. Twenty years of research on cytokine-induced sickness behavior. Brain Behav Immun 2007;21:153-60. [Crossref] [PubMed]
- Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 1999;99:2192-217. [Crossref] [PubMed]
- Brook RD, Appel L, Rubenfire M, et al. Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the American heart association. Hypertension 2013;61:1360-83. [Crossref] [PubMed]
- Bradt J, Dileo C, Potvin N. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane database Syst Rev 2013;12:CD006577 [Crossref] [PubMed]
- Grissom GR, Phillips RA. Screening for depression: this is the heart of the matter. Arch Intern Med 2005;165:1214-6. [Crossref] [PubMed]
- Dal Lin C, Tona F, Osto E. The crosstalk between the cardiovascular and the immune system. Vasc Biol 2019;1:H83-8. [Crossref] [PubMed]
- Dal Lin C, Silvestro M, Migliorini R, et al. Integrated Approach to Arrhythmias. In: Integrative Cardiology. Cham: Springer International Publishing, 2017:237-45.
- Dal Lin C, Silvestro M, Migliorini R, et al. Integrated Approach to Heart Failure. In: Integrative Cardiology. Cham: Springer International Publishing, 2017:223-35.
- Dal Lin C, Silvestro M, Migliorini R, et al. Integrated Approach to Coronary Artery Disease. In: Integrative Cardiology. Cham: Springer International Publishing, 2017:203-21.
- Dal Lin C, Silvestro M, Migliorini R, et al. Integrated Approach to Hypertension. In: Integrative Cardiology. Cham: Springer International Publishing, 2017:185-201.
- Piccoli M, Fioranelli M, Roccia MG, et al. Integrated Approach to Dyslipidemia. In: Integrative Cardiology. Cham: Springer International Publishing, 2017:175-84.
- Fioranelli M, Del Prete M, Aracena JC, et al. Low-Dose Therapy for the Treatment of Low-Grade Chronic Inflammation. In: Integrative Cardiology. Cham: Springer International Publishing, 2017:27-38.
- Dal Lin C, Tona F, Osto E. Coronary Microvascular Function and Beyond: The Crosstalk between Hormones, Cytokines, and Neurotransmitters. Int J Endocrinol 2015;2015:312848 [Crossref] [PubMed]
- Dal Lin C, Marinova M, Rubino G, et al. Thoughts modulate the expression of inflammatory genes and may improve the coronary blood flow in patients after a myocardial infarction. J Tradit Complement Med 2017;8:150-63. [Crossref] [PubMed]
- Castillo-Richmond A, Schneider RH, Alexander CN, et al. Effects of stress reduction on carotid atherosclerosis in hypertensive African Americans. Stroke 2000;31:568-73. [Crossref] [PubMed]
- Schneider RH, Alexander CN, Staggers F, et al. A randomized controlled trial of stress reduction in African Americans treated for hypertension for over one year. Am J Hypertens 2005;18:88-98. [Crossref] [PubMed]
- Razavi M, Fournier S, Shepard D, et al. Effects of lifestyle modification programs on cardiac risk factors. PLoS One 2014;9:e114772 [Crossref] [PubMed]
- Ornish D, Scherwitz LW, Billings JH, et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA 1998;280:2001-7. [Crossref] [PubMed]
- Gould KL, Ornish D, Scherwitz L, et al. Changes in myocardial perfusion abnormalities by positron emission tomography after long-term, intense risk factor modification. JAMA 1995;274:894-901. [Crossref] [PubMed]
- Ornish D, Lin J, Chan JM, et al. Effect of comprehensive lifestyle changes on telomerase activity and telomere length in men with biopsy-proven low-risk prostate cancer: 5-year follow-up of a descriptive pilot study. Lancet Oncol 2013;14:1112-20. [Crossref] [PubMed]
- Ornish D, Brown SE, Scherwitz LW, et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet 1990;336:129-33. [Crossref] [PubMed]
- Dal Lin C, Gola E, Brocca A, et al. miRNAs may change rapidly with thoughts: The Relaxation Response after myocardial infarction. Eur J Integr Med 2018;20:63-72. [Crossref]
- Dal Lin C, Grasso R, Scordino A, et al. Ph, Electric Conductivity and Delayed Luminescence Changes in Human Sera of Subjects Undergoing the Relaxation Response: A Pilot Study. Preprints 2020. doi:
10.20944/PREPRINTS202004.0202.V1 . - Rosenkranz MA, Jackson DC, Dalton KM, et al. Affective style and in vivo immune response: neurobehavioral mechanisms. Proc Natl Acad Sci U S A 2003;100:11148-52. [Crossref] [PubMed]
- Irwin MR, Olmstead R, Oxman MN. Augmenting immune responses to varicella zoster virus in older adults: a randomized, controlled trial of Tai Chi. J Am Geriatr Soc 2007;55:511-7. [Crossref] [PubMed]
- Leserman J, Jackson ED, Petitto JM, et al. Progression to AIDS: the effects of stress, depressive symptoms, and social support. Psychosom Med 1999;61:397-406. [Crossref] [PubMed]
- Romeo J, Warnberg J, Pozo T, et al. 3rd International Immunonutrition Workshop Session 6: Role of physical activity on immune function Physical activity, immunity and infection Proceedings of the Nutrition Society Proceedings of the Nutrition Society. Proc Nutr Soc 2010;69:390-9. [Crossref] [PubMed]
- Committee on Military Nutrition Research, Institute of Medicine. Military Strategies for Sustainment of Nutrition and Immune Function in the Field. National Academy Press, Washington, D.C, 1999.
- Winkler ES, Thackray LB. A long-distance relationship: the commensal gut microbiota and systemic viruses. Curr Opin Virol 2019;37:44-51. [Crossref] [PubMed]
- Read SA, Obeid S, Ahlenstiel C, et al. The Role of Zinc in Antiviral Immunity. Adv Nutr 2019;10:696-710. [Crossref] [PubMed]
- Vetvicka V, Vetvickova J. Immune-enhancing effects of Maitake (Grifola frondosa) and Shiitake (Lentinula edodes) extracts. Ann Transl Med 2014;2:14. [PubMed]
- Balkrishna A, Pokhrel S, Singh J, et al. Withanone from Withania somnifera May Inhibit Novel Coronavirus (COVID-19) Entry by Disrupting Interactions between Viral S-Protein Receptor Binding Domain and Host ACE2 Receptor. Virol J 2020; [Crossref]
- Yang Y, Islam MDS, Wang J, et al. Traditional Chinese medicine in the treatment of patients infected with 2019-new coronavirus (SARS-CoV-2): A review and perspective. Int J Biol Sci 2020;16:1708-17. [Crossref] [PubMed]
- Cinatl J, Morgenstern B, Bauer G, et al. Glycyrrhizin, an active component of liquorice roots, and replication of SARS-associated coronavirus. Lancet 2003;361:2045-6. [Crossref] [PubMed]
- Dharmendra M, Deepak S. Evaluation of Traditional Ayurvedic Preparation for Prevention and Management of the Novel Coronavirus (SARS-CoV-2) Using Molecular Docking Approach. chemRxiv 2020.
- Thaker PH, Han LY, Kamat AA, et al. Chronic stress promotes tumor growth and angiogenesis in a mouse model of ovarian carcinoma. Nat Med 2006;12:939-44. [Crossref] [PubMed]
- Chida Y, Hamer M, Wardle J, et al. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat Clin Pract Oncol 2008;5:466-75. [Crossref] [PubMed]
- Lutgendorf SK, Sood AK. Biobehavioral factors and cancer progression: physiological pathways and mechanisms. Psychosom Med 2011;73:724-30. [Crossref] [PubMed]
- Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer 2009;115:5349-61. [Crossref] [PubMed]
- Pinquart M, Duberstein PR. Associations of social networks with cancer mortality: a meta-analysis. Crit Rev Oncol Hematol 2010;75:122-37. [Crossref] [PubMed]
- Andersen BL, Yang HC, Farrar WB, et al. Psychologic intervention improves survival for breast cancer patients: a randomized clinical trial. Cancer 2008;113:3450-8. [Crossref] [PubMed]
- Witek-Janusek L, Albuquerque KC, Chroniak KR, et al. Effect of mindfulness based stress reduction on immune function, quality of life and coping in women newly diagnosed with early stage breast cancer. Brain Behav Immun 2008;22:969-81. [Crossref] [PubMed]
- Cirillo N, Prime SS. Keratinocytes synthesize and activate cortisol. J Cell Biochem 2011;112:1499-505. [Crossref] [PubMed]
- Arck PC, Slominski A, Theoharides TC, et al. Neuroimmunology of stress: skin takes center stage. J Invest Dermatol 2006;126:1697-704. [Crossref] [PubMed]
- Chapman BP, Moynihan J. The brain-skin connection: role of psychosocial factors and neuropeptides in psoriasis. Expert Rev Clin Immunol 2009;5:623-7. [Crossref] [PubMed]
- van der Mei IAF, Ponsonby AL, Dwyer T, et al. Past exposure to sun, skin phenotype, and risk of multiple sclerosis: case-control study. BMJ 2003;327:316. [Crossref] [PubMed]
- Acheson ED, Bachrach CA, Wright FM. Some comments on the relationship of the distribution of multiple sclerosis to latitude, solar radiation, and other variables. Acta Psychiatr Scand Suppl 1960;35:132-47. [Crossref] [PubMed]
- Sospedra M, Martin R. Immunology of multiple sclerosis. Annu Rev Immunol 2005;23:683-747. [Crossref] [PubMed]
- Buljevac D, Hop WCJ, Reedeker W, et al. Self reported stressful life events and exacerbations in multiple sclerosis: prospective study. BMJ 2003;327:646. [Crossref] [PubMed]
- Bierhaus A, Wolf J, Andrassy M, et al. A mechanism converting psychosocial stress into mononuclear cell activation. Proc Natl Acad Sci U S A 2003;100:1920-5. [Crossref] [PubMed]
- Bottaccioli F. Il sistema immunitario: la bilancia della vita, II edizione. Tecniche Nuove 2008.
- Straub RH, Dhabhar FS, Bijlsma JWJ, et al. How psychological stress via hormones and nerve fibers may exacerbate rheumatoid arthritis. Arthritis Rheum 2005;52:16-26. [Crossref] [PubMed]
- Sharpe L, Sensky T, Timberlake N, et al. Long-term efficacy of a cognitive behavioural treatment from a randomized controlled trial for patients recently diagnosed with rheumatoid arthritis. Rheumatology (Oxford, England) 2003;42:435. [Crossref] [PubMed]
- Kjeldsen-Kragh J, Haugen M, Borchgrevink CF, et al. Controlled trial of fasting and one-year vegetarian diet in rheumatoid arthritis. Lancet 1991;338:899-902. [Crossref] [PubMed]
- Peralta-Ramírez MI, Jiménez-Alonso J, Godoy-García JF, et al. The effects of daily stress and stressful life events on the clinical symptomatology of patients with lupus erythematosus. Psychosom Med 2004;66:788-94. [Crossref] [PubMed]
- Greco CM, Rudy TE, Manzi S. Effects of a stress-reduction program on psychological function, pain, and physical function of systemic lupus erythematosus patients: a randomized controlled trial. Arthritis Rheum 2004;51:625-34. [Crossref] [PubMed]
- Rosenkranz MA, Davidson RJ, Maccoon DG, et al. A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation. Brain Behav Immun 2013;27:174-84. [Crossref] [PubMed]
Cite this article as: Dal Lin C, Ferrari F, Zampieri F, Tona F, Osto E. From traditional Mediterranean, Ayurvedic and Chinese medicine to the modern time: integration of pathophysiological, medical and epistemological knowledge. Longhua Chin Med 2020;3:21.

