Placebo and food cravings control: results from two randomized controlled trials
Introduction
Food cravings (FC) refer to an intense desire to eat specific types of foods (1); this has been linked to body mass index (BMI) and consumption of sweet, high-fat, carbohydrate/starches and fast-food in community-dwelling individuals (2). Although FC do not reflect abnormal eating behavior per se, very intense and frequent experiences are associated with obesity and eating disorders such as bulimia nervosa and binge eating disorder (3).
In this respect, FC in unsuccessful dieters or restrained eaters have been related to a lack of control over eating, and keeping up consuming daily planning (4), which altogether represent a problem whenever individuals need to overcome daily temptations by the mere use of their own willpower (5). It seems that such individuals may need some sort of tool to bridge the gap between intention and action.
About two decades ago, the Homeopathic Pharmacy of Santa Clara (Cuba) began delivering a Bach Flower Remedies (BFR)-formula which claimed helped individuals lose weight. Many people attributed its effect to the fact that it was easier for them to control their “anxiety to eat”. In addition, a recent study in Brazil showed that overweight and obese individuals did perceive benefits from an intervention with BFR on both self-control and anxiety reduction (6).
In Cuba, we speak of “anxiety to eat” meaning FC rather than referring to an emotion which leads to eating (7). FC could then so be considered as a major problem among overweight and obese Cuban adults (8). The potential of using BFR in helping individuals with eating disorders or obesity has been previously suggested as a helping tool for them (9,10), but no known research up to date has yet investigated whether BFR can truly help individuals or not in controlling their FC.
Systematic reviews agree that BFR are essentially a placebo (11-13); even more, a useful one (12,14-16). It is important to highlight that although recent studies have shown specific effects (17-22) we consider the majority of responses to BFR in clinical practice as a broad collection of spurious therapeutic effects (23).
In fact, it has been suggested that spirituality could be the main dispositional predictor of the effect of BFR (24-27). Furthermore, it has also been suggested that spirituality predicts self-opinion about BFR whenever individuals receive enough information about this therapy, regardless of their dispositional optimism, or whether they have or not already received treatment (28).
This kind of meaning response has been used to interpret those placebo responses (29,30) in which patients respond to a pharmacologically inert treatment (31). In some cases, it has been observed a Goldilocks placebo effect when individuals have chosen their own BFR-formula among some other “correct” number of options (32).
Following the idea that there is a wide applicability for psychological interventions to be delivered in conjunction with complementary and alternative medicines (CAM) approaches, as a part of an overall health maintenance strategy (33), we hereby submit two studies which evaluate the effectiveness of a BFR-formula in controlling FC.
Study 1 consisted in a double-blind placebo-controlled trial aimed to assess the specific effect of the suggested formula and the overall effectiveness of the placebo-control in individuals with high trait FC. Beyond blinding and randomization, we consider mandatory controlling both Spirituality (34)—because BFR already are a kind of a spiritualized therapy (24), and Expectancy regarding treatment efficacy (35)—because expectancy is a given predictive factor of placebo responses (36). As it has been stated above, we can only attribute differential improvements to the potential of the treatment (37) when the active control group has reached the same expectation of improvement (and spirituality for current studies) as the experimental group.
Study 2 combined an implementation intention instruction with the BFR-formula aimed to reduce FC in overweight and obese adults while at home. Implementation intention is an ‘if-then’ plan, which defines exactly when, where, and how one wants to act towards one’s own goals (38). It has been considered a useful resource for those individuals committed to self-control of FC (39,40). In this context, the use of replacements provide them with an alternative action instead of suppressing or ignoring the cue (41). This study did not involve deception, because uncertainty about treatment allocation could also affect the response to the intervention when compared with common clinical practice (42,43). The suitability to combine psychological techniques with acupressure in order to ameliorate FC had been previously tested (44). Thus, the combination of CAM with psychological interventions could provide proactive strategies to reduce FC and obesity, via interventions not explicitly oriented towards weight loss (45).
Study 1: a useful placebo
Objectives, design and hypothesis
Study 1’s main purpose was to evaluate both the specific effects attributed to the BFR-formula, and the overall effectiveness of the placebo intervention in order to control FC on individuals with frequent and intense experiences of FC in their everyday life. Reductions in BMI were also assessed as a secondary goal in order to provide an objective and clinically important outcome measure.
In order to investigate on these objectives, we applied a 3×3 mixed factorial design. The within-subject factor was “time”, with three measurement points (baseline, 1 month later and 3 months later). The between-subject factor was “group” with BFR group, along with Placebo group and Control group. Participants were randomized as they picked a number from 1 to 3 from a bowl after the baseline assessment: 1= BFR group; 2= Placebo group; 3= Control group.
It was hypothesized that BFR and Placebo group would experience reductions in trait FC due to intervention. Furthermore, it was also hypothesized that results in both groups would eventually show a greater reduction in trait FC, even a greater one than that of Control group, because of the meaning associated to treatment.
Participants
The current research was approved by the Scientific Council of the Faculty of Psychology at the Universidad Central “Marta Abreu” de Las Villas (UCLV, Cuba); project number 33/11-12. It was conducted between January and July 2012, and written consent was obtained from all participants. It was carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
There were 196 participants, recruited from a large sample of 1,241 adults coming from a prior Study (7) (exclusion criteria included pregnancy, lactation, elderly population, active eating disorders, or any other diagnosed psychopathological disorder). Advertisements sought ‘‘individuals who are experiencing strong FC in their everyday life and would like to reduce them”.
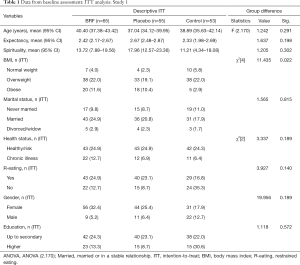
For these individuals to be recruited, they had to score over percentile 75 (total score ≥159) in the Food Craving Questionnaire Trait—valid for Cuban adults (46). Advertisements were posted on several family physicians’ offices billboards pertaining to the authors’ institutions where individuals were being assessed, emphasizing the fact that the intended intervention was not just to go on a diet and target to reduce FC. Characteristics of the different groups during the baseline assessment are shown in Table 1. All participants voluntarily accepted to participate in the study and no monetary compensation was offered to them.
Full table
Measures
Socio-demographic/anthropometric and clinical data: Participants were asked to give out their age; gender; height; education level; marital status and current weight.
Restrained eating was assessed using one single item question: “Do you often restrain your food intake to reduce or maintain your weight?” (Yes/No).
Food Cravings Questionnaire-Trait: the Spanish version of such questionnaire (7,47) measures the intensity of nine trait FC dimensions (see Table 2). Instructions ask participants to reveal how frequently each given statement “would be true for you in general”, using a 6-point scale that ranged from 1 (never or not applicable) to 6 (always).
Full table
Spiritual Connection Questionnaire: consists of 14 items regarding the experience of a spiritual connection with the Universe and with other people, and the happiness such connection brings to one-self (48). Responses were scored on a Likert scale ranging from –3 (does not describe me at all) to 3 (it fully describes me).
Expectancy: “At this point of time, do you expect intervention to help you?”. Responses were scored on scale ranging from –3 (unlikely it will help) to 3 (definitely think it will help).
At follow-up (3 months later), an additional question was posed in order to analyze the desire to continue with the intervention: “Would you like to continue using this resource?” (Yes/No/I’m not sure). Lastly, researchers also kept a record of the number of bottles delivered to BFR and Placebo group participants, and added the following compliance question: “On average, how many times a day did you take the given formula?” Answers were ranging from 0= “never” to 6= “in accordance with the prescription”.
Procedure
The current Study consisted of three basic stages: (I) baseline (pre-intervention); (II) post-intervention (1 month after baseline); and (III) follow-up (3 months after baseline).
Baseline: first of all, the specific objectives of the Study were explained and consent forms were given out and then duly signed. Three trained psychologists managed sociodemographic and clinical measures, assessed FC, spirituality, and measured height and weight (BMI), all at the physician’s office. Afterwards, participants were randomly allocated to either BFR, Placebo or Control group by their correspondent psychologist, and were given out their own proper instructions (see below).
Post-intervention: 1 month later, each participant returned to the physician’s office and his/her assigned psychologist measured his/her weight and assessed trait FC again. Follow-up: 3 months after baseline final measures of weight and trait FC were taken by the assigned psychologist. By the end of the 3rd month participants were also asked the questions described in the following section regarding their particular perceived difficulty to control FC and their desire to continue using the suggested intervention. Upon completion, participants were thanked for their participation.
BFR formula was prepared by the Homeopathic Pharmacy of Santa Clara. Included remedies were chosen because of their purported action on self- control and cravings (Agrimony, Cherry Plum, Walnut, White Chestnut and Crab Apple) (49). Neither participants nor field researchers were aware of the formula composition. Recommended dosage was 4 drops every 4 hours approximately taken between 7 am and 22 pm: BFR = alcohol 10% + BFR; Placebo = alcohol 10%.
Researchers were commissioned to provide participants of BFR group with free bottles of the formula throughout all 3 months intervention lasted. BFR, Placebo and their corresponding instructions were delivered by the assigned psychologist right after each participant’s allocation. Psychologists were trained by the lead BFR researcher. Participants from both groups were informed that BFR formula would help them control their FC. On the other hand, Control group participants were given a single instruction which appealed to their intention to control FC: “You will do your best to control your cravings and your thoughts about food using your willpower” (5).
Analyses were conducted on both groups per-protocol (PP) and intention-to-treat (ITT) samples (those who did not take the formula at least four times a day were considered non-compliant and were included only in the ITT analysis). Nonetheless, just for the sake of parsimony, PP analyses were reported only where results differed from the ITT analysis. Data analysis was performed using the SPSS/Windows (version 20). Changes in trait FC and BMI were assessed using a mixed ANOVA (GLM for repeated measures); groups were assessed as between-subject factor; measurements were assessed as within-subject factor. Effect sizes were calculated using partial Eta squared (), where values above 0.01; 0.06 and 0.14 were interpreted as the effect of small, medium and large, respectively (50). To test whether the formula had or not specific effects, we compared BFR and Placebo groups. Thus, to test the effectiveness of the placebo response associated to BFR meaning, we compared Placebo and Control group. T-tests were conducted in order to determine between-group differences. Effect sizes were calculated using Cohen’s d, where values above 0.2; 0.5 and 0.8 were interpreted as the effect of small, respectively (50). Group comparisons for nominal data were conducted using chi-square.
Results and final discussion
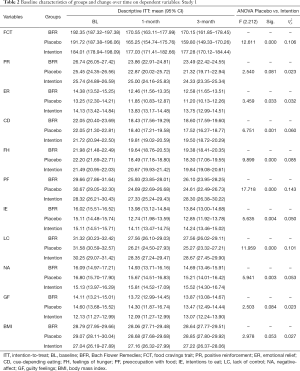
Participants flow through the experiment, as well as the reasons for exclusion, are all depicted on Figure 1A.
Baseline assessment
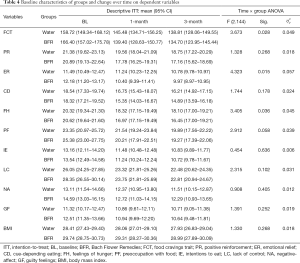
As may be seen on Table 1, groups did not differ in age, spirituality, education, marital and health status, or restrained eating. Nevertheless, there were observed differences for gender and BMI classification. In the latter case, the observed imbalance might be caused by many obese participants declining to continue in the study once they were assigned to Control group.
Although female participants were majority in each group, there were more men in Control group. However, it is important to point out that 13 out of 15 participants from this group who withdrew from the study were women. Men seem more prone than women to believing in their “willpower” to control FC.
Along the same line, significant differences between groups were observed for trait FC [F (2.170) =3.508, P=0.032, =0.040], although their effect size was small. This difference was caused by participants from the Control group who withdrew from the study, and who showed mean values on trait FC [208.02 (179.25–188.91)] higher than those who completed the study (see Table 2) [t (66) =4.697, P<0.01, d=1.44]. This selective attrition has also been observed in therapy, where individuals who do not improve are more likely to leave the process (23).
BFR vs. Placebo
The effect of Time was significant for the overall trait FC and the majority of its dimensions with reductions over time and large effect sizes [FITT (2.236) between 22.147 and 62.194, P<0.001 and between 0.146 and 0.345], with the exception of negative affect [FITT (2.236) =12.124, P<0.001, =0.093] and guilty feelings [FITT (2.236) =1.030, P=0.359]. However, the effect size of Time on BMI could be considered very small [FITT (2.236) =3.707, P=0.026, =0.030]. Finally, PP analysis showed the largest effect sizes for trait FC and all its dimensions [FPP (2.90) between 16.998 and 106.573, P<0.001 and between 0.274 and 0.703] and BMI [FPP (2.236) =7.427, P=0.001, =0.142].
Regarding time × group, results were in line with previous findings (11-13) with absence of significant between-group differences for most variables [FITT (2.236) between 0.196 and 2.976, not significant (NS)] with the exception of preoccupation with food [FITT (2.236) =3.425, P=0.034, =0.028] and lack of control over eating [FITT (2.236) =3.177, P=0.044, =0.026] where, surprisingly, Placebo showed better results than BFR (see Table 2). These differences disappeared with PP analysis, but displaying a new one favorable to Placebo group for feelings of hunger [FPP (3.297) =3.177, P=0.041, =0.068] (Figure 1B). These results may be explained by the transactional model of placebo responding (see General discussion) (51) as well as the likelihood that BFR might be captive of its own meaning (30,52).
ITT and PP revealed no significant between-group differences for desire to continue, number of bottles and compliance. ITT analysis showed that 55% of participants (n=65) wished to continue with the intervention, consumed approximately one bottle (30 mL) per month and took the formula at least twice a day. On the other hand, PP analysis revealed that 76% of participants (n=36) wished to continue with the intervention and took the formula at least five times a day.
Intention to control FC: various responses to a single instruction
Results within Control group revealed significant reductions for trait FC, positive reinforcement, feelings of hunger, intention to eat, lack of control over eating with medium effect sizes [F (2.104) between 3.588 and 7.488, P<0.035 and between 0.065 and 0.126]. A larger and positive effect size was observed for cue-dependent eating [F (2.104) =19.099, P<0.001 and =0.269]. Table 2 shows slight increases from the 1st to the 3rd month of the follow-up; this could be an indicator of will weakness to attain a certain goal by using a mere intention instruction (38). As time passes by, an increasing number of intervening events can reduce the predictive validity of intentions on behavior (53).
On the other hand, it was observed a paradoxical increase of guilty feelings with a medium effect size [F (2.104) =4.245, P<0.020 and =0.075], but not an increase of preoccupation with food and negative affect [F (2.104) <1.3, NS]. A parallel study showed paradoxical effects on these FC dimensions with large effect sizes among overweight and obese individuals after receiving the same instruction and follow-up (5). These differences might be explained by the inclusion of normal weight individuals in spite their experiencing frequent and intense FC. Thus, responses to an intention instruction to control FC seemed to be positive for most dependent variables. Finally, slight and not significant increases in BMI through both follow-ups highlighted the futility of the intention (in absence of additional resources) to achieve weight control on most participants.
Placebo vs. Intention
Because researchers were interested on testing placebo response, analysis was focused on time × group. ITT analysis revealed significant differences on most dependent variables, with the exception of positive reinforcement, guilty feelings and BMI (Table 2). Effect sizes were large for preoccupation with food and medium for trait FC, cue-dependent eating and lack of control over eating. On the other hand, PP analysis showed significant differences for all dependent variables [FPP (2.148) between 5.463 and 44.765, P<0.005] with large effect sizes for most variables [between 0.148 and 0.377] but guilty feelings (=0.107) and BMI (=0.069).
Reductions in Placebo group should be considered quite impressive as we bear in mind lower scores for trait FC in Control group, mainly caused by participants who withdrew the study after baseline assessment. Results on BMI should be analyzed with caution due to the fact that many obese participants declined to continue in the intervention after allocation in Control group.
Conclusions
Although BFR-formula did not show any extra effects over Placebo formula, responses to intervention observed on both groups showed reductions of trait FC, and had major effects on large effect size, especially among compliant participants. Furthermore, significant between group-differences favorable to Placebo group were observed for preoccupation with food and for lack of control over eating which suggested an increased response associated with the meaning of the intervention. Third, responses to placebo showed highest effectiveness on trait FC, preoccupation with food, cue-dependent eating and lack of control over eating. Finally, response to the meaning of BFR intervention seemed to be a suitable approach to control FC on individuals who showed very intense and frequent FC experiences on their everyday life.
Study 2: implementing a placebo replacement
Objectives, design and hypothesis
The objective of this study was to evaluate the effectiveness of an implementation intention instruction using BFR in order to reduce FC on overweight and obese individuals. Reductions in BMI were also assessed as a secondary objective in order to provide an objective and clinically important outcome measure.
A mixed factorial design was applied (see Study 1), although with BFR and Water groups as the between-subject factor. Design did not involve deception, and participants were informed as to what they were getting. Participants were randomized to either BFR or control (Water) group by allocation of a number based on arrival sequence (even numbers were assigned to BFR group).
Firstly, it was hypothesized that both groups would experience reductions in trait FC, because both groups received the implementation intention instruction, as well as direct instructions to consume water, which could reduce stress (54) and provide relief from FC. Secondly, it was hypothesized that those with BFR diluted into water would have greater reduction in trait FC rather than control over it, because of the meaning associated with treatment.
Participants
This study was conducted between February and October 2012 right after having obtained both institutional approval and written consent from all participants; it is project number 33/11-12. This study has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
Participants were 74 individuals who responded to our recruiting advertisements and who fulfilled the inclusion criteria (see Study 1). Advertisements sought “overweight or obese people, who are experiencing strong cravings for food when they are at home and would like to reduce these cravings”.
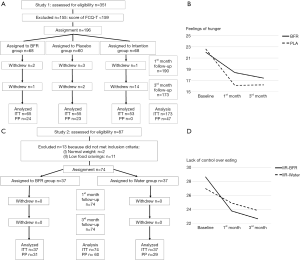
For individuals to be selected, they had to report strong and frequent (more than once a day) FC at home. Advertisements were posted on several family physicians’ offices billboards pertaining to the authors’ institutions, emphasizing the fact that the intended intervention was not just to go on a diet and that it just targeted to replace an unhealthy snacking habit. Characteristics of BFRs and Water groups are shown in Table 3. All participants voluntarily accepted to participate in the study and no compensation was offered to them.

Full table
Measures
Study 1: socio-demographic/anthropometric and clinical data; Food Cravings Questionnaire-Trait; Spiritual Connection Questionnaire; restrained eating; expectancy, and desire to continue at follow-up.
At follow-up (3 months later) an additional question was included, in order to analyze the perceived difficulty for FC self-control: was it difficult for you to control your FC using the assigned resource? Scores ranged from 1 (very difficult to achieve) to 9 (very easy to achieve). Participants were asked to keep a daily record about how many times a day they used the assigned replacement.
Procedure and data analysis (see Study 1)
Implementation intention instructions
Both groups received the same initial instruction: “between regular meals, if I am at home and I feel an intense desire to eat; instead of taking a snack I will drink sips of the replacement over a 20-minute period”. The BFR group was instructed to sip from a glass of water with the BFR solution diluted into it (Study 1): the recommended dosage was 4 drops per glass of water. BFR participants were informed that BFR formula would help them control their FC. Water group was informed that sips of water would help them reduce their FC. All participants were instructed to follow this program at least once a day during a 90 days period of time; those who reported not having followed this protocol were considered non-compliant participants.
Results and discussion
The flow of participants through the experiment, including reasons for exclusion, is depicted on Figure 1C.
Baseline assessment
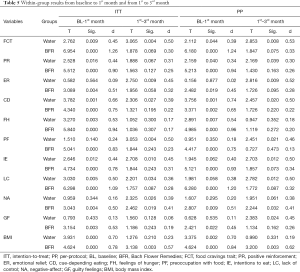
As can be seen in Table 3, groups did not differ throughout all assessed variables. No significant differences between groups were observed for BMI, FC trait and all its dimensions [tITT (72) between 0.253 and 1.897 and tPP (58) between 0.009 and 1.185; NS].
Effectiveness of the intervention
Time effect was significant for the overall FC trait with a reduction in FC score over time [FITT (2.144) =48.826, P<0.001 and =0.404] as well as for all its dimensions [FITT (2.144) between 10.008 and 43.837, P<0.001]. Effects were large for lack of control over eating (=0.378), feelings of hunger (=0.344), cue-dependent eating (=0.342), intention to eat (=0.300), positive reinforcement (=0.294), preoccupation with food (=0.241) and emotional relief (=0.147). Medium to large effect sizes were observed for negative affect (=0.131) and guilty feelings (=0.122).
Positive outcomes seemed to rely precisely on intentionally programming their minds to automatically trigger favorable responses when whichever critical cue might be encountered (55). Provided the reported problems related to self-control in relation to overeating, these findings indicated that implementation intentions may be useful translating a goal intention into action (38) and reducing hedonic hunger (56). As a concurrent task, focusing one’s mind on drinking sips of water could diminish the captivating power of everyday temptations (57).
There was a significant reduction of BMI over time with large effect size [FITT (2.144) =26.311, P<0.001 and =0.268]. Both replacements appeared to be helpful for weight reduction, perhaps as a result of a more successful control of their FC.
Table 4 presents time × group interactions (using ITT), where the highest score reductions were observed in the BFR group for the FC trait, emotional relief and feelings of hunger. Effects could be classified from small to medium, and emotional relief showed the largest effect size (=0.057). Most results were replicated when using PP analysis except for lack of control over eating [F (2.116) =4.023, P=0.020, =0.065] where the BFR participants had significantly lower scores than Water participants (Figure 1D). BFR have been historically used by health practitioners to correct emotional imbalances (12,58). Thus, drinking sips of BFR diluted into water may be a useful way for individuals to achieve emotional relief beyond eating their desired food.
Full table
Additional questions at follow-up
Table 3 shows additional assessments on dependent variables at follow-up. On ITT analysis both groups used replacement formula approximately once per day, but Water group reported a more perceived difficulty on FC self-control than BFR group, with a medium effect size (see Table 5). PP analysis showed similar results (d=0.58). Regarding participants desire to maintain in the future the usage of the assigned replacement, answers tended to be affirmative for both groups. However, a significant number of Water group individuals were hesitant about continuing with the use of intervention habits thereinafter.
Full table
The meaning behind BFR treatment (26) as well as its associated therapeutic ritual (59), might have contributed to deliver better outcomes for BFR group. Thus, unconscious activation of inhibitory control mechanisms (60) might be the pathway through which individual’s control over eating improves (when taking BFR). Likewise, the effect of performing the so explained ritual consisting on diluting BFR into water should also be considered as an explanatory factor to observed outcomes for this particular group (59).
The current study has contributed to the understanding (and application) of implementation intentions on everyday life. Although the fact that a simple implementation intention might have such effects could be striking, it is important to highlight here that FC seem to be reduced as well whenever individuals are distracted with carrying another task such as working with clay (61), playing Tetris (62) or even taking a brisk walk (63), instead of trying to suppress it (64,65).
Conclusions
To conclude, we can state that implementation intention instruction intervention had positive effects on FC as well as BMI. Adding BFR into water was more effective in controlling the anticipation of relief as a result of eating, and in controlling the lack of control over eating. All enhanced outcomes in BFR group could be explained by placebo mechanisms, in which meaning and rituals pertaining treatment may contribute to obtaining better outcomes.
General discussion
In the current paper, we analyzed the effect of BFR both on a standalone basis and combined with an implementation intention instruction on FC control. Results from both studies highlight the response to BFR meaning. Moreover, it shows that interventions were sufficiently appealing as most participants, with the exception of Control group, wished to continue with their assigned resource. These effects could be mainly attributed to the meaning of the intervention, in view of the results observed in Placebo group, all consistent with systematic reviews (11-13).
Unexpected significant differences favorable to placebo in Study 1 might suggest an increased meaning effect (29). Taking into account BFR’s underlying philosophy, very similar to Homeopathy (33), they could be considered as an expanded mind/body therapy from a health psychology point of view. As it has been previously highlighted, some CAM could be captive of the efficacy paradox (30).
However, transactional model of placebo responding suggests an interesting framework for managing future research studies, and for interpreting, current differences between BFR and Placebo groups. For instance, BFR effects on reducing FC could also be considered as a placebo response, and be explained by trait reward sensitivity factors. Prior researches have shown these last ones to be significantly related to FC (66) and to placebo responding (67), due to individuals responding differently to the various aspects of the treatment (51). Whereas on an outwardly oriented point of view, dopamine sensitive individuals may have responded to the treatment because of its perceived novelty, on an inward oriented one, serotonin sensitive individuals may have responded to the suggestion by focusing on their internal states.
Thus, the match between an individual’s biological trait-like response system and his personal environmental contingencies (51) may determine magnitude of the placebo response to any identical placebo. A recent transcultural study on Cubans and Italians showed differences in their reward sensitivity factor (68), considering the main features on the appetitive system (69), for both food rationing and food-availability. Remember food restrictions were imposed as a part of general rationing of goods among Cubans in their everyday life, whereas this had not been a factor for Italians.
Overall, findings indicate that BFR could be a useful placebo in the context of controlling food related thoughts, reducing hunger, providing relief from negative emotional states, and promoting self-control over eating as a response to external cues. These findings have increasing relevance in a context where cue-dependent eating and lack of control over eating are better attributes of BMI among all assessed dimensions of trait FC (8).
CAM are recommended as ethical placebos in primary health care (69). Given proof of placebos ability to exert neurobiological effects (70), these approaches are a feasible way of translating the ‘power of placebo’ for improving patient care (71,72), in the same way the use of BFR can help individuals overcome their FC.
One of the major strengths of the study is the fact that it encourages the application of placebo in clinical practice, as well as implementation intentions in an everyday life. Furthermore, participants were recruited from the general population and results were assessed on the 3rd month of follow-up. Last, there were conducted ITT and PP analysis. It is important to highlight the fact that researchers used active control conditions, and matched expectancy and spirituality as predictors of placebo responses (37).
However, the study’s contribution should also be considered in light of its limitations. To begin with, although the current study included a follow-up assessment, longer-term follow-up should be needed to be able to discern lasting effects. Secondly, clinical and psychopathological diagnoses were retrieved from medical records, and did not involve further analysis for corroboration. Thirdly, our investigation was mainly based on self-reported measures, which may be biased due to social desirability. To end with, it should be pointed out the unbalance observed in Study 1 during after baseline assessment for trait FC, BMI and gender in Control group, all of which weakened favorable changes over time among placebo participants in between-group comparisons.
To conclude, there was no evidence that supports specific effects for BFR on FC control beyond its meaning. However, the intended interventions had positive effects on trait FC and were more effective in controlling preoccupation with food, feelings of hunger, cue-dependent eating and lack of control over eating. Additionally, results suggest that implementation intentions may be a useful tool for delivering BFR in everyday life, as it is very easy to use at home, and there is an indication that effects may last at least in the medium term. Such interventions could be efficiently delivered through the use of different technologies (73) as a self-help placebo intervention. Moreover, it could be used as a complementary resource for FC control either on interventions not explicitly oriented toward weight loss (45) or on scalable weight loss treatment in primary care (74) always provided there is motivational concordance between the individual and the suggested resource (24).
Acknowledgments
We are truly grateful to Michael E. Hyland and Ben Whalley for their support during the design of the study. We are also indebted with Margot Darragh, Adrian Meule and Isabelle Mack for their helpful comments and suggestions on earlier versions of this paper. Finally, we would like to thank María Infiesta for language correction.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/lcm-2009-006). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The current research was approved by the Scientific Council of the Faculty of Psychology at the Universidad Central “Marta Abreu” de Las Villas (UCLV, Cuba); project number 33/11-12. Written consent was obtained from all participants. It was carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kemps E, Tiggemann M. A cognitive experimental approach to understanding and reducing food cravings. Curr Dir Psychol Sci 2010;19:86-90. [Crossref]
- Chao A, Grilo CM, White MA, et al. Food cravings, food intake, and weight status in a community-based sample. Eat Behav 2014;15:478-82. [Crossref] [PubMed]
- Rodríguez-Martín BC, Meule A. Food craving: new contributions on its assessment, moderators, and consequences. Front Psychol 2015;6:21. [PubMed]
- Meule A, Lutz A, Vögele C, et al. Food cravings discriminate differentially between successful and unsuccessful dieters and non-dieters. Validation of the food cravings questionnaires in German. Appetite 2012;58:88-97. [Crossref] [PubMed]
- Rodríguez-Martín BC, Gómez-Quintana A, Díaz-Martínez G, et al. Bibliotherapy and food cravings control. Appetite 2013;65:90-5. [Crossref] [PubMed]
- Pancieri AP, Fusco SB, Ramos BIA, et al. Meanings of flower therapy for anxiety in people with overweight or obesity. Rev Bras Enferm 2018;71:2310-5. [Crossref] [PubMed]
- Rodríguez-Martín BC, Molerio-Pérez O. Exploring the factor structure of the Food Cravings Questionnaire-Trait in Cuban adults. Front Psychol 2014;5:214. [PubMed]
- Rodríguez-Martín BC, Gil-Pérez P, Pérez-Morales I. Exploring the "weight" of food cravings and thought suppression among Cuban adults. Eat Weight Disord 2015;20:249-56. [Crossref] [PubMed]
- Simonetta M. Experience with Bach Flower Therapy in a group of patients with eating disorders. Eur J Integr Med 2012;4:116. [Crossref]
- Mehta SK. Oral flower essences for ADHD. J Am Acad Child Adolesc Psychiatry 2002;41:895-author reply 895-6. [Crossref] [PubMed]
- Ernst E. Bach flower remedies: a systematic review of randomised clinical trials. Swiss Med Wkly 2010;140:w13079 [PubMed]
- Halberstein RA, Sirkin A, Ojeda-Vaz MM. When less is better: a comparison of Bach Flower Remedies and homeopathy. Ann Epidemiol 2010;20:298-307. [Crossref] [PubMed]
- Thaler K, Kaminski A, Chapman A, et al. Bach Flower Remedies for psychological problems and pain: a systematic review. BMC Complement Altern Med 2009;9:16. [Crossref] [PubMed]
- Walach H, Rilling C, Engelke U. Efficacy of Bach-flower remedies in test anxiety: a double-blind, placebo-controlled, randomized trial with partial crossover. J Anxiety Disord 2001;15:359-66. [Crossref] [PubMed]
- . Howard J. Do Bach flower remedies have a role to play in pain control? A critical analysis investigating therapeutic value beyond the placebo effect, and the potential of Bach flower remedies as a psychological method of pain relief. Complement Ther Clin Pract 2007;13:174-83. [PubMed]
- Rodríguez Martín BC, Rivas Suárez SR. Placebo: la «mancha» más brillante de la Medicina. Revista Cubana de Investigaciones Biomédicas 2013;32:366-78.
- Rivas Suárez S, Valido Díaz A, Blanco Machado F. Estudio preclínico del efecto de las esencias florales de Bach en la inflamación aguda. Revista Cubana de Investigaciones Biomédicas 2013;32:65-73.
- Rodríguez Martín BC. Esencias Florales de Bach: efecto del White Chestnut sobre los pensamientos intrusos indeseados. Revista Cubana de Investigaciones Biomédicas 2012;31:0-0.
- Turrini RNT. Clinical trial with Bach Flower Remedies to evaluate their effect on the spiritual well-being of Brazilian university students with common mental disorders. Eur J Integr Med 2012;4:185. [Crossref]
- Rivas-Suárez SR, Águila-Vázquez J, Suárez-Rodríguez B, et al. Exploring the effectiveness of external use of Bach Flower Remedies on carpal tunnel syndrome: a pilot study. J Evid Based Complementary Altern Med 2017;22:18-24. [Crossref] [PubMed]
- Resende MM, Costa FE, Gardona RG, et al. Preventive use of Bach flower Rescue Remedy in the control of risk factors for cardiovascular disease in rats. Complement Ther Med 2014;22:719-23. [Crossref] [PubMed]
- Yang S, Wang Y. P02. 177. Effects of Bach Rescue remedy on cardiac autonomic balance in healthy women. BMC Complement Altern Med 2012;12:233. [Crossref]
- Lilienfeld SO, Ritschel LA, Lynn SJ, et al. Why ineffective psychotherapies appear to work: a taxonomy of causes of spurious therapeutic effectiveness. Perspect Psychol Sci 2014;9:355-87. [Crossref] [PubMed]
- Hyland ME. Motivation and placebos: do different mechanisms occur in different contexts? Philos Trans R Soc Lond B Biol Sci 2011;366:1828-37. [Crossref] [PubMed]
- Hyland ME, Geraghty AW, Joy OE, et al. Spirituality predicts outcome independently of expectancy following flower essence self-treatment. J Psychosom Res 2006;60:53-8. [Crossref] [PubMed]
- Hyland ME, Whalley B. Motivational concordance: an important mechanism in self-help therapeutic rituals involving inert (placebo) substances. J Psychosom Res 2008;65:405-13. [Crossref] [PubMed]
- Hyland ME, Whalley B, Geraghty AW. Dispositional predictors of placebo responding: a motivational interpretation of flower essence and gratitude therapy. J Psychosom Res 2007;62:331-40. [Crossref] [PubMed]
- Rodríguez-Martín BC, Fallas-Durán M, Gaitskell B, et al. Predictors of positive opinion about Bach Flower Remedies in adults from three Latin-American countries: an exploratory study. Complement Ther Clin Pract 2017;27:52-6. [Crossref] [PubMed]
- Moerman DE. Against the "placebo effect": a personal point of view. Complement Ther Med 2013;21:125-30. [Crossref] [PubMed]
- Walach H. Placebo controls: historical, methodological and general aspects. Philos Trans R Soc Lond B Biol Sci 2011;366:1870-8. [Crossref] [PubMed]
- Benedetti F, Amanzio M. Mechanisms of the placebo response. Pulm Pharmacol Ther 2013;26:520-3. [Crossref] [PubMed]
- Hafner RJ, White MP, Handley SJ. The Goldilocks placebo effect: placebo effects are stronger when people select a treatment from an optimal number of choices. Am J Psychol 2018;131:175-84. [Crossref]
- Nezu CM, Tsang S, Lombardo ER, et al. Complementary and alternative therapies. In: Weiner IB. editor. Handbook of psychology. New York: Whiley, 2003:591-614.
- Hyland ME, Masters KS, Wheeler P, et al. A sense of ‘special connection’, self-transcendent values and a common factor for religious and non-religious spirituality. Archive for the Psychology of Religion 2010;32:293-326. [Crossref]
- Colagiuri B. Participant expectancies in double-blind randomized placebo-controlled trials: potential limitations to trial validity. Clin Trials 2010;7:246-55. [Crossref] [PubMed]
- Horing B, Weimer K, Muth ER, et al. Prediction of placebo responses: a systematic review of the literature. Front Psychol. 2014;5:1079. [Crossref] [PubMed]
- Boot WR, Simons DJ, Stothart C, et al. The pervasive problem with placebos in psychology: why active control groups are not sufficient to rule out placebo effects. Perspect Psychol Sci 2013;8:445-54. [Crossref] [PubMed]
- Gollwitzer PM. Weakness of the will: is a quick fix possible? Motiv Emot 2014;38:305-22. [Crossref]
- May J, Andrade J, Panabokke N, et al. Images of desire: cognitive models of craving. Memory 2004;12:447-61. [Crossref] [PubMed]
- Achtziger A, Gollwitzer PM, Sheeran P. Implementation intentions and shielding goal striving from unwanted thoughts and feelings. Pers Soc Psychol Bull 2008;34:381-93. [Crossref] [PubMed]
- Adriaanse MA, Gollwitzer PM, De Ridder DT, et al. Breaking habits with implementation intentions: a test of underlying processes. Pers Soc Psychol Bull 2011;37:502-13. [Crossref] [PubMed]
- Roy J. Randomized treatment-belief trials. Contemp Clin Trials 2012;33:172-7. [Crossref] [PubMed]
- Enck P, Klosterhalfen S. The placebo response in clinical trials-the current state of play. Complement Ther Med 2013;21:98-101. [Crossref] [PubMed]
- Stapleton P, Sheldon T, Porter B, et al. A randomised clinical trial of a meridian-based intervention for food cravings with six-month follow-up. Behaviour Change 2011;28:1-16. [Crossref]
- Bacon L, Aphramor L. Weight science: evaluating the evidence for a paradigm shift. Nutr J 2011;10:9. [Crossref] [PubMed]
- Rodríguez Martín BC, Molerio-Pérez O, Abreu-Cervantes A, et al. Cuestionarios del Ansia por la Comida. In: Rodríguez-Martín BC, Molerio-Pérez O, Rodríguez-Alonso L, et al. Valdación de Instrumentos Psicológicos: Criterios Básicos. Santa Clara: Feijóo, 2012:13-24.
- Cepeda-Benito A, Gleaves DH, Fernández MC, et al. The development and validation of Spanish versions of the State and Trait Food Cravings Questionnaires. Behav Res Ther 2000;38:1125-38. [Crossref] [PubMed]
- Wheeler P, Hyland ME. The development of a scale to measure the experience of spiritual connection and the correlation between this experience and values. Spirituality and Health International 2008;9:193-217. [Crossref]
- Orozco R. Flores de Bach, 38 descripciones dinámicas. Barcelona: El Grano de Mostaza Ediciones, 2010.
- Sink CA, Mvududu NH. Statistical power, sampling, and effect sizes: three keys to research relevancy. Counseling Outcome Research and Evaluation 2010;1:1-18. [Crossref]
- Darragh M, Booth RJ, Consedine NS. Who responds to placebos? Considering the "placebo personality" via a transactional model. Psychol Health Med 2015;20:287-95. [Crossref] [PubMed]
- Kirsch I. The placebo effect revisited: lessons learned to date. Complement Ther Med 2013;21:102-4. [Crossref] [PubMed]
- Ajzen I. The theory of planned behaviour: reactions and reflections. Psychol Health 2011;26:1113-27. [Crossref] [PubMed]
- Forshaw MJ, Jones SJ. A test of the properties of a proprietary complementary remedy in conditions of temporary, induced, cognitive stress. Perfusion 2010;23:14-7.
- Hofmann W, Kotabe H. A general model of preventive and interventive self-control. Soc Personal Psychol Compass 2012;6:707-22. [Crossref]
- Witt AA, Raggio GA, Butryn ML, et al. Do hunger and exposure to food affect scores on a measure of hedonic hunger? An experimental study. Appetite 2014;74:1-5. [Crossref] [PubMed]
- Van Dillen LF, Papies EK, Hofmann W. Turning a blind eye to temptation: how cognitive load can facilitate self-regulation. J Pers Soc Psychol 2013;104:427-43. [Crossref] [PubMed]
- Williamson EM, Rankin-Box D. Complementary therapies, the placebo effect and the pharmacist. Complement Ther Clin Pract 2009;15:172-9. [Crossref] [PubMed]
- Kaptchuk TJ. Placebo studies and ritual theory: a comparative analysis of Navajo, acupuncture and biomedical healing. Philos Trans R Soc Lond B Biol Sci 2011;366:1849-58. [Crossref] [PubMed]
- Hepler J, Albarracin D. Complete unconscious control: using (in)action primes to demonstrate completely unconscious activation of inhibitory control mechanisms. Cognition 2013;128:271-9. [Crossref] [PubMed]
- Andrade J, Pears S, May J, et al. Use of a clay modeling task to reduce chocolate craving. Appetite 2012;58:955-63. [Crossref] [PubMed]
- Skorka-Brown J, Andrade J, May J. Playing 'Tetris' reduces the strength, frequency and vividness of naturally occurring cravings. Appetite 2014;76:161-5. [Crossref] [PubMed]
- Oh H, Taylor AH. A brisk walk, compared with being sedentary, reduces attentional bias and chocolate cravings among regular chocolate eaters with different body mass. Appetite 2013;71:144-9. [Crossref] [PubMed]
- Erskine JA. Resistance can be futile: investigating behavioural rebound. Appetite 2008;50:415-21. [Crossref] [PubMed]
- Erskine JA, Georgiou GJ. Effects of thought suppression on eating behaviour in restrained and non-restrained eaters. Appetite 2010;54:499-503. [Crossref] [PubMed]
- Franken IH, Muris P. Individual differences in reward sensitivity are related to food craving and relative body weight in healthy women. Appetite 2005;45:198-201. [Crossref] [PubMed]
- Scott DJ, Stohler CS, Egnatuk CM, et al. Individual differences in reward responding explain placebo-induced expectations and effects. Neuron 2007;55:325-36. [Crossref] [PubMed]
- Rodríguez-Martín BC, Innamorati M, Imperatori C, et al. Eating behaviors in Cuban adults: results from an exploratory transcultural study. Front Psychol 2016;7:1455. [Crossref] [PubMed]
- Howick J, Bishop FL, Heneghan C, et al. Placebo use in the United kingdom: results from a national survey of primary care practitioners. PLoS One 2013;8:e58247 [Crossref] [PubMed]
- Benedetti F, Mayberg HS, Wager TD, et al. Neurobiological mechanisms of the placebo effect. J Neurosci 2005;25:10390-402. [Crossref] [PubMed]
- Colloca L, Miller FG. Harnessing the placebo effect: the need for translational research. Philos Trans R Soc Lond B Biol Sci 2011;366:1922-30. [Crossref] [PubMed]
- Colloca L, Jonas WB, Killen J, et al. Reevaluating the placebo effect in medical practice. Z Psychol 2014;222:124-7. [Crossref] [PubMed]
- Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspect Psychol Sci 2011;6:21-37. [Crossref] [PubMed]
- Barnes RD, White MA, Martino S, et al. A randomized controlled trial comparing scalable weight loss treatments in primary care. Obesity (Silver Spring) 2014;22:2508-16. [PubMed]
Cite this article as: Rodríguez-Martín BC, Frías-Hernández LM, O’Farril-Jiménez JC, Guillén-Verano ÁM, Pastorrecio-González L, Chinea-Monzón Y, O’Farril-Rodríguez MC, Cartalla-Gálvez MJ, Águila-Vega CA, Molina-Santos I, Hernández-Rodríguez I. Placebo and food cravings control: results from two randomized controlled trials. Longhua Chin Med 2020;3:1.