Traditional Japanese medicine in geriatrics, evidences and the guideline
Geriatric syndrome
Geriatric syndromes include a number of conditions typical of, if not specific to, aging, such as dementia, depression, delirium, incontinence, vertigo, falls, spontaneous bone fractures, failure to thrive, and neglect and abuse. Geriatric syndromes are associated with reduced life expectancy. To be considered a geriatric syndrome, these conditions must interfere with a person’s daily life.
Here, we introduce some evidences of traditional Chinese medicine for geriatric syndrome and clinical practice guideline from Japan Geriatrics Society. How can we treat geriatric syndrome using traditional Chinese Medicine?
Dementia
Despite a small sample size and a short observation period, we demonstrated that a combinatorial use of donepezil plus kamiuntanto, KUT was more beneficial than donepezil alone in both cognition and brain perfusion (Figure 1). Therefore, it is likely that donepezil and KUT worked synergistically in a safe fashion to enhance an availability of acetylcholine (1).

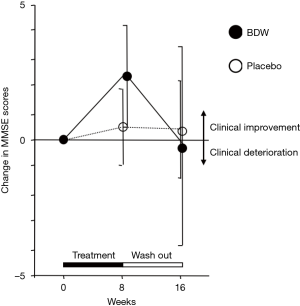
Sametime, we showed that bawei dihuan wang (BDW) could improve the cognitive function of Alzheimer disease patient. Figure 2 shows that BDW improves Mini Mental Score Examination about 2.5 in the treatment period (2).
Traditional Chinese medicine for behavioral and psychological symptoms of dementia (BPSD)
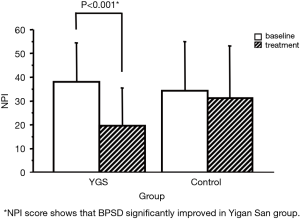
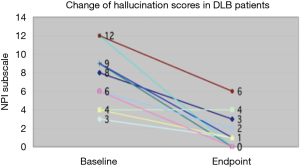
BPSD is the serious clinical problem of geriatric syndrome. We reported that Yigan San could improve BPSD without extrapyramidal side effects causing by major tranquilizers (Figure 3) (3). At the same time, we also found that Yigan San could improve typical hallucination in Dementia with Lewy Bodies (DLB), as shown in Figure 4 (4).
Aspiration pneumonia
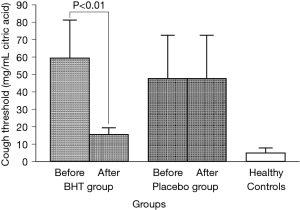
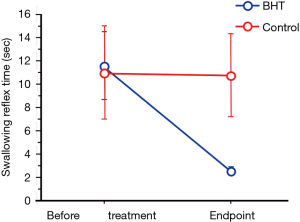
Pneumonia is now the third reason of death of Japanese, and most of them are aspiration pneumonia in the elderly. Absence or attenuation of the cough (5) and swallowing (6) reflex is shown in elderly patients with aspiration pneumonia. We investigated the effects of a traditional Chinese medicine Banxia Houpo Tang (BHT, Hange Koboku-To in Japanese, formula magnolia et pinelliae), on the swallowing (7) (Figure 5) and cough (8) (Figure 6) reflexes in elderly stroke patients. Finally, we found that BHT reduced pneumonia risk in the elderly (Figure 7) (9). The BHT group was able to maintain self-feeding better than the control group (P=0.006).
Chronic constipation
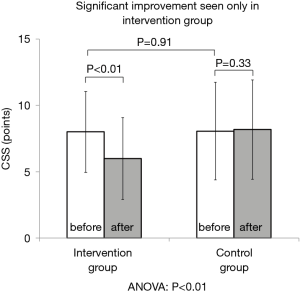
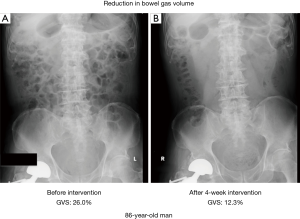
There were over 1.34 million patients suffering from cerebrovascular diseases in 2008 reported by Ministry of Health, Labour and Welfare in Japan. Constipation is one of the complications seen in poststroke patients (10). Japanese medicine Daikenchuto (DKT) improved chronic constipation of poststroke patients. Poststroke patients with functional constipation, assessed by the Rome III criteria, from 6 hospitals were recruited in a study on the effects of the traditional Japanese medicine Daikenchuto (DKT) on constipation. The total score on the Constipation Scoring System (CSS) improved significantly by DKT (Figure 8). The Gas volume score was also significantly reduced in the DKT group compared to the control (Figure 9, P=0.03) (11).
Guideline
Concerning these evidences, Japan Geriatric Society treated traditional medicine as the independent chapter in their guideline 2015 (12). As a result, Yigan San, Banxia houpu Tang, Dajianzhong Tang, Buzhongyiqi Tang, and Ma Zi Ren Wan covering by Japanese national insurance, were reviewed and found to have a high Quality of evidence for the elderly (Table 1).

Full table
Conclusions
As mentioned above, evidences of traditional medicine for geriatrics accumulated little by little, and a part of it is accepted modern medical doctors. But Japan luck of systematic educational system for traditional medicine, causing irrelevant usage. Nation wide systematic system of education, study, and medical care are required.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/lcm.2019.09.01). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Maruyama M, Tomita N, Iwasaki K, et al. Benefits of combining donepezil plus traditional Japanese herbal medicine on cognition and brain perfusion in Alzheimer's disease: a 12-week observer-blind, donepezil monotherapy controlled trial. J Am Geriatr Soc 2006;54:869-71. [Crossref] [PubMed]
- Iwasaki K, Kobayashi S, Chimura Y, et al. A randomized, double-blind, placebo-controlled clinical trial of the Chinese herbal medicine "ba wei di huang wan" in the treatment of dementia. J Am Geriatr Soc 2004;52:1518-21. [Crossref] [PubMed]
- Iwasaki K, Satoh-Nakagawa T, Maruyama M, et al. A randomized, observer-blind, controlled trial of the traditional Chinese medicine Yi-Gan San for improvement of behavioral and psychological symptoms and activities of daily living in dementia patients. J Clin Psychiatry 2005;66:248-52. [Crossref] [PubMed]
- Iwasaki K, Maruyama M, Tomita N, et al. Effects of the Traditional Chinese Herbal Medicine for Cholinesterase inhibitor-Resistant Visual Hallucinations and Neuropsychiatric Symptoms in patients with Dementia with Lewy Bodies. J Clin Psychiatry 2005;66:1612-3. [Crossref] [PubMed]
- Sekizawa K, Ujiie Y, Itabashi S, et al. Lack of cough reflex in aspiration pneumonia. Lancet 1990;335:1228-9. [Crossref] [PubMed]
- Nakazawa H, Sekizawa K, Ujiie Y, et al. Risk of aspiration pneumonia in the elderly. Chest 1993;103:1636-7. [Crossref] [PubMed]
- Iwasaki K, Wang Q, Nakagawa T, et al. The Traditional Chinese Medicine Banxia Houpo Tang improves swallowing reflex. Phytomedicine 1999;6:103-6. [Crossref] [PubMed]
- Iwasaki K, Cyong JC, Kitada S, et al. A traditional Chinese herbal medicine, banxia houpo tang, improves cough reflex of patients with aspiration pneumonia. J Am Geriatr Soc 2002;50:1751-2. [Crossref] [PubMed]
- Iwasaki K, Kato S, Monma Y, et al. A pilot study of banxia houpu tang, a traditional Chinese medicine, for reducing pneumonia risk in older adults with dementia. J Am Geriatr Soc 2007;55:2035-40. [Crossref] [PubMed]
- Su Y, Zhang X, Zeng J, et al. New-onset constipation at acute stage after first stroke: incidence, risk factors, and impact on the stroke outcome. Stroke 2009;40:1304-9. [Crossref] [PubMed]
- Numata T, Takayama S, Tobita M, et al. Traditional Japanese medicine daikenchuto improves functional constipation in poststroke patients. Evid Based Complement Alternat Med 2014;2014:231258.
- Takayama S, Iwasaki K. Systematic review of traditional Chinese medicine for geriatrics. Geriatr Gerontol Int 2017;17:679-88. [Crossref] [PubMed]
Cite this article as: Iwasaki K. Traditional Japanese medicine in geriatrics, evidences and the guideline. Longhua Chin Med 2019;2:13.